December 15, 2020
Your mouth: It's good for talking, kissing, and (most importantly) chewing and assimilating delicious food so you can nourish your body—nothing groundbreaking there. But did you ever stop to think about the microbiome of your mouth? Yes, you may be surprised to read that your mouth has a microbiome of its own, one that is intimately bound to your endocrine, immune, and digestive systems.
Just like your gut microbiome (which I covered in this article), your mouth is host to a thriving bacterial community, on which your overall health greatly depends—and whose balance is the key to vitality in your mouth and entire body alike.
Unfortunately, many of the periodontal procedures and medications of modern dentistry disrupt the beneficial bacteria of your gums and mutate your mouth’s microbes. This is why, despite brushing twice daily, flossing, and regular dentist visits, a staggering number of cavities are drilled and filled, root canals are performed, and teeth are yanked from our bodies. Something is clearly amiss. In fact, 91% of Americans over 20 have had cavities at some point in their lives and 27% of adults over 20 have untreated cavities.
So, for today's article—a guest post by Nadine Artemis, who joined me on the podcast “Is Charcoal Toothpaste OK, 8 Crucial Mouth Beauty & Oral Health Tips, Peptides For Oral Care, The Invisible Dental Flow In Your Mouth & Much More.“—you'll discover how to combat the triple threat that is sabotaging the health of your gaping maw: a poor understanding of the tooth-nurturing dentinal fluid, harmful dental procedures, and the periodontal scorched-earth policy on bacteria. You'll also learn simple steps you can take to prepare your mouth for a dental appointment, how to make your own natural dental care products at home, and much more.
The Invisible Toothbrush
Your teeth are fed through their roots by the dentinal-lymph system, in which lymph liquid spins inward and upward into your teeth's core, the pulp chamber, then flows through your teeth and out onto your enamel.
This microscopic flow of fluid originates near your intestines and flows through your teeth like microscopic sweat—flushing out toxins, providing nutrients for your teeth’s mineral matrix, and repelling microbial biofilm (a thin, slimy film made up of single-cell organisms that, together, act more like a larger, multi-celled organism) on your tooth surfaces, which prevents tooth decay and gum disease.
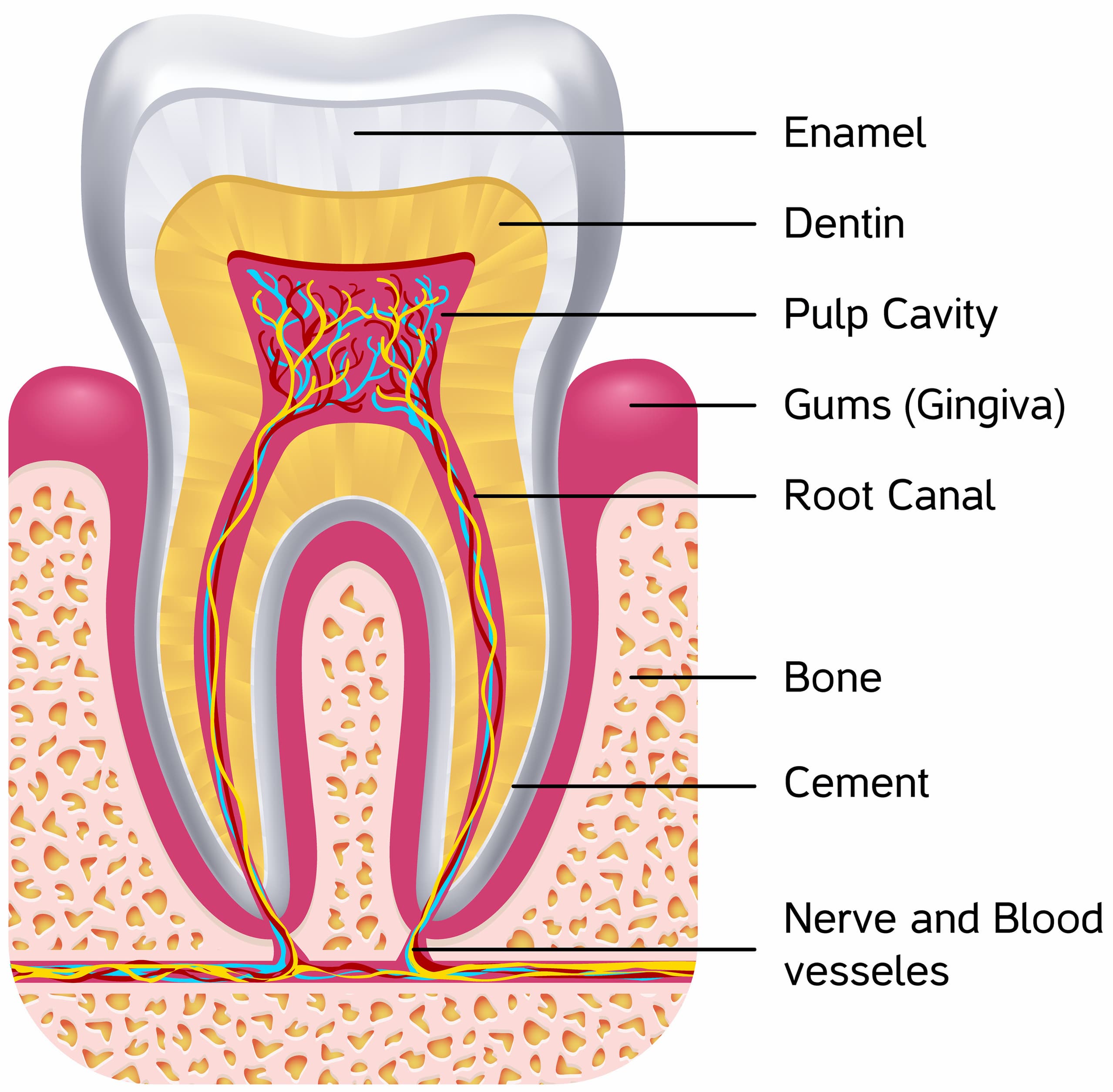
When this dentinal-lymph secretion is properly metabolized and functional, it acts as an invisible toothbrush, preventing systemic decay, inhibiting the penetration of pathogens, and neutralizing acids on your teeth's surfaces. However, this dentinal-lymph flow can stagnate and even fully reverse. When this happens, the capillaries in your teeth suck in bacteria like a straw and cause infection and biofilm formation within the pulp chamber and dentin tubules. This self-contaminating system causes a “leaky tooth,” and it is the genesis of cavity creation.
A cavity is an infection in the tooth, and, like all wounds, they have the ability to heal. Your teeth are alive, and the current condition of your teeth and mouth can evolve with proper care and nutrition. Dr. Ralph R. Steinman, the same dentist who scientifically proved the existence of the dentinal-lymph system, showed that including dietary magnesium and phosphorus reduced the tooth decay rate by 86 percent. Dr. Melvin Page confirmed this by finding that when phosphorus blood levels drop below 3.5, cavities begin to form.
What causes magnesium and phosphorus levels to drop?
Food grown on mineral-depleted soils has led to magnesium-depleted food and widespread magnesium deficiencies. You can take a deep dive into everything magnesium by listening to Ben's podcast “Magnesium Supplementation: Everything You Need To Know About Dosing Magnesium, Timing Magnesium, Forms Of Magnesium & More!” As for phosphorus, healthy kidneys keep blood serum phosphorus between 3.4 to 4.5 mg/dl. This range is so delicate that your body will steal phosphorus from your teeth and bones to keep the serum levels from dropping below 3.4. Fluctuations within the normal range can occur and are typically caused by age (phosphorus levels are higher in children than in adults), time of day, nutrition, and health status. Unlike magnesium, phosphorus is abundant in nutritious foods and rarely needs supplementation in people who eat a variety of colorful, organic foods. Extended fasting, vomiting, diarrhea, heavy use of antacids, excessive calcium (>2500mg/day), and alcohol abuse are a few common factors that create conditions for blood phosphorus levels to drop below 3.4.
For more information on dietary minerals, check out Ben’s podcast with Barton Scott: The Problem With Mineral Supplements, Why Minerals Don’t Get Absorbed, Why You Probably Have A Mineral Deficiency & What To Do About It.
When the underlying causes of cavities are addressed and dentinal-lymph flow is restored, teeth will remineralize and become more resilient to cavities in the future. Fillings are nothing more than Band-Aid solutions that are susceptible to recurrent decay and present a host of other issues you're about to discover.
Detrimental Dental Procedures
Modern dental procedures—including dental amalgams, root canals, and wisdom teeth removal—can also be detrimental to oral health and mutate your oral microbes.
Let's start with dental amalgams.
Made from a combination of silver, copper, tin, and mercury, dental amalgams have been used to fill cavities for more than 150 years. They are far more economical and durable than other filling materials, and because they are easier to place than composite fillings, the ADA recommends them for children. You're about to learn why this is a big problem.
Aside from requiring your dentist to drill away healthy bone to prepare your tooth, these eighteenth-century dental solutions are 50 percent mercury, one of the most toxic substances on the planet.
Even though this toxicity is scientific fact, many traditional dentists continue to use mercury fillings. A cumulative toxin that passes through the blood-brain and placental barriers, mercury tenaciously binds to tissue, altering DNA, nerves, cell membranes, and mitochondrial function. As author James Wynbrandt reports in The Excruciating History of Dentistry: Toothsome Tales & Oral Oddities from Babylon to Braces, mercury toxicity is linked to dementia, multiple sclerosis, Parkinson’s, and other degenerative disorders. Mercury has also been linked to periodontal disease, receding gums, and skin hyperpigmentation.
The U.S. Environmental Protection Agency (EPA) claims that the highest body-burden of chronic mercury toxicity comes from silver fillings. In addition, when mercury fillings are removed, even though there is not a metallurgic change to the mercury, the EPA considers it toxic waste, and fillings must be handled with a strict no-touch protocol to protect dentists and the environment from mercury poisoning. The FDA states, “A person with four fillings has enough mercury to make a 20-acre lake unfit for fishing.” Yet, somehow, it is still okay for our mouths and tongues to touch it daily, and it is still not universally banned in dentistry. Both old and new mercury fillings release vapors twenty-four hours a day, with a 500% increase when chewing, teeth grinding, and drinking hot fluids. According to the Journal of Dental Research, gum chewing increases mercury-vapor release considerably!
For more on heavy metal toxicity (and detoxification), and what to do about it, check out some of the following podcasts of Ben's:
- How Hidden Sources Of Heavy Metals Are Destroying Your Health, And What You Can Do About It.
- The Crucial Do’s And Don’ts Of Heavy Metal Testing And Metal Detoxification.
- Special Episode: How I’m Going To Completely Detox My Body In 2018 (Detox Myths Busted, Detox 101, Advanced Detox Strategies & Much More!)
- The Most Effective Detox You’ve Never Heard Of (And Exactly How To Do It).
Next up is the root canal, a procedure for an infected tooth that kills the tooth by removing its internal structure, including the nerves, pulp tissue, and blood vessels. The hollowed-out tooth is rinsed, filled with latex and cement, and then topped with a crown.
The purpose of a root canal is to hermetically seal the tooth and save the chewing surface. Theoretically, this seems like a good idea; clinically, it is a bacterial horror story. The whole goal of a root canal is to have a noninfected, sterile tooth, but the exact opposite often happens.
After a root canal, the dead tooth remains in the mouth as an incubator of infection, a bacterial breeding ground, and a necrotic nest for pathogens to grow and spread. Each tooth contains three miles of microscopic dentin tubules that are impossible to sterilize. With the blood vessels removed, neither antibiotics nor white blood cells can reach the location to fight infection. Every time a root-canaled tooth is used to chew, bacterial toxins are squirted into the bloodstream. These toxins that flow from the anaerobic infection silently spread to the gums, ligaments, and jawbone. Because the nerve tissue is removed in the procedure, there will be no pain indicating infection.
Dr. Stuart Nunnally, a highly respected and pioneering biological dentist, conducted independent tests on root-canaled teeth. To qualify, the teeth had to be symptom-free and show zero signs of pathology on an X-ray. One hundred percent of these root-canaled teeth, upon surface inspection and in X-rays, were textbook-perfect root canals, yet lab tests revealed that the teeth harbored severe toxic pathogens. While this type of information has not yet permeated into every dental practice (with this knowledge comes some ethical decisions for dentists about how to approach diseased teeth), thankfully there is vibrant discussion in endodontics journals about the impossibility of sterility in root-canal-treated teeth.
If you have a root canal and this information is unnerving, it is important to know this: Although root canals become focal infections that feed anaerobic bacteria 100% of the time, not all root canals cause systemic health issues (because of an individual’s epigenetics and because each person handles toxicity differently).
If you are experiencing a decline in health (especially in the months preceding the procedure), or if you have an autoimmune issue, you may want to explore having root-canaled teeth extracted and the periodontal ligament removed. This is an easier decision if it is a back molar, as the space can be left as is, but a more difficult decision with a front tooth, as you may then need to explore a bridge or a zirconium post-implant tooth. Titanium posts are commonly used, though they may deposit alloys and ions in the surrounding tissues that can lead to inflammation, bone loss, and implant failure.
Finally, there is the unnecessary process of removing wisdom teeth. It is common dentistry practice to extract these molars as prophylactic prevention to avoid impacted teeth and because partially erupted wisdom teeth may be hard to clean or may affect neighboring teeth.
The good news is that some researchers are beginning to ask if it is wise to remove these molars. A report published in the American Journal of Public Health deemed that 6.7 million out of 10 million preventive wisdom tooth extractions are unnecessary. The British National Health Service has stated that the practice of prophylactic removal of pathology-free impacted wisdom teeth should be discontinued. There is insufficient evidence that impacted wisdom teeth cause problems, and the expense and risks of the surgery are not justified. Additionally, wisdom teeth extraction can also alter the structure of one's neck, jaw, and mouth and may change the shape of the face.
But that’s not all.
Multiple pathological bacteria are often found in the jaw on wisdom-tooth extraction sites. This is because it is standard protocol to leave the soft periodontal ligament in after extraction. This leftover ligament causes a sluggish area in the bone marrow where virulent bacteria gather and eat away at the jawbone, creating cavitations (an area of infection, inflammation, or necrosis within the jawbone). These jaw cavitations are a hidden consequence of wisdom-teeth extractions, as most of the time, there are no visible symptoms. When a jaw cavitation shows up on an X-ray, the bone has already eroded by 50 percent. These areas in the jaw are medically referred to as osteonecrotic lesions. Dr. Hal Huggins’s research institute revealed that these jaw-cavitation sites are sanctuaries for serious pathogens that can lead to an array of autoimmune diseases.
Dentists can check for cavitations by making a small incision in the gum of the extraction site and examining for mushy pockets in the jawbone. If there is decay, a simple procedure can clear it up: The site is opened, the decay is scraped off the bone, bacteria are thoroughly removed, blood flow to the area is re-established, and the site is treated with ozone. If you do need a tooth extracted, including a wisdom tooth, be sure to work with a dentist who will also be sure to remove the periodontal ligament as part of the protocol. You'll learn more in the summary about how to find qualified biological dentists in your area.
Fortunately, more and more dentists are beginning to question these detrimental dental procedures, and there are new frontiers in dentistry that can help rectify the damage already caused. Some biological dentists use platelet-rich plasma (PRP) therapy to stimulate growth factors and ozone injections and gels to clean infections and infuse surgical sites with a “breath of fresh air.” These dentists are also leading the way with more biocompatible material choices. Dentists who are leading the field with these innovations will be among the first to integrate successful stem-cell therapy for tooth regeneration, which will be a reality in the very near future.
Your Mouth's Microbial Menagerie
There are about as many bacteria in your mouth as there are people on the planet. Your mouth is a microbial menagerie, and as a holobiont human host to these microbes, you share an elaborate evolutionary and ancient alliance.
As a good host, you provide a stable, loving home and nourishing food for your flora friends. In return, these microbes micromanage your body by digesting food and secreting beneficial biochemicals. They are also sentient sentinels that strengthen your immunity while preventing pathogenic periodontal party-crashers from proliferating and from excreting endotoxins and colonizing the healthy community.
The key to oral health is maintaining an ecologically balanced and diverse microbiome. Contrary to this, we have been caught in the dross of carpet-bombing the biome—practicing a scorched-earth policy of periodontal care: chemicals in teeth bleaching, fillings, rinses, and fluoride; sudsy surfactants in toothpastes; antibiotic atomic bombs on bacteria; masticating meals of glyphosates and pesticides; root canals festering focal infections; metallic masses of mercury, titanium, and nickel.
Just as toxic food and chemical irritants induce leaky guts by microscopically perforating the intestines, the scrubbing and rubbing of your gums with medicants and caustic chemicals can cause leaky gums. Bacteria from your mouth do not normally enter the bloodstream, but dental procedures and products can perforate the epithelium (the skin in your mouth that is only one cell thick), providing a port of entry into your bloodstream. When the bacteria and plaque that cause tooth decay and gum disease enter your circulatory system, they cause a cascade of inflammation, releasing cytokines and C-reactive proteins.
Antibiotics are often prescribed for oral infections—even though they fail to penetrate biofilm—and contribute to mutating the balance of your mouth’s microbiome. Antibiotics are indiscriminate assassins. Any surviving resistant bacteria mutate fast and bask in the empty niches the antibiotics made. Soon, pathogenic biofilms bloom, and you no longer have protection from infection.
Healthy mouths contain a certain population of pathogens; the goal is to have the good bacteria far outnumber the bad. Normally, pathogens exist in a free-floating planktonic state in your body’s ecosystem, but when they grow in numbers, they are able to gain traction by communicating, thus enabling them to colonize into a biofilm. Under healthy conditions, an oral-ecological balance of bacteria keeps biofilms healthy and stable. Dental plaque is an ideal nest for germs, so you need a dental care strategy that inhibits bacterial communications that create biofilms, while at the same time balances bacteria in lieu of destroying the microbiome. You'll discover some of these mouth microbiome optimizing strategies below.
How To Elevate Your Oral Ecology
With just a few updates to your oral care and health routine, you can significantly elevate your oral health. At the end of this section, you'll find recipes for creating your own natural toothpaste, tooth serum, and mouthwash.
To support a healthy oral ecology, remember the following three words: Stop, Seal, and Seed, which Ben and I discuss in detail on the podcast we recorded, “Is Charcoal Toothpaste OK, 8 Crucial Mouth Beauty & Oral Health Tips, Peptides For Oral Care, The Invisible Dental Flow In Your Mouth & Much More With Nadine Artemis.“
The first step is to STOP the daily habits that are compromising your healthy oral ecology. Whatever improvements you make to your mouth will also benefit your whole-body well-being.
- Stop phytic acid consumption. Phytic acid is an antinutrient that plunders cavity-preventing phosphorus stores in your body. Soak and ferment gluten-free grains, legumes, and nuts to reduce this antinutrient.
- Stop spikes in blood sugar: Ben's article “5 Simple Steps You Can Take To Live Longer, Banish Blood Sugar Swings & Massively Enhance Energy Levels.” has some good tips on controlling blood sugar.
- Stop eating the endocrine inhibitors of processed food, sugar, gluten, corn, and glyphosate irritants.
- Stop mouth breathing.
- Stop the microbe mutators of excessive antibiotics, glyphosates, surfactants, and fluoride toothpastes.
- Have a qualified biological dentist who follows the removal procedures of the Hal Huggins Institute remove your mercury fillings. (Information on finding a biological dentist is provided in the summary.)
- Stop using synthetic tooth-cleaning products. If toothpaste is such a magical teeth cleaner, then why are cavities at an all-time high, and why do most toothpastes come with a big warning label: “May be harmful if swallowed”? It is best to be a purist about oral health and diligently care for your teeth using natural products such as the ones you'll discover at the end of this section.
Next, SEAL leaky gums by restoring integrity to your oral epithelium. Bleeding, inflamed, and receding gums are signs of bacterial imbalance, and that bacteria may be entering your bloodstream.
- Seabuckthorn, rose otto, frankincense, and myrrh essential oils—diluted in a lipid, such as coconut or MCT oil—are all vulnerary “botanical-biotics” known for their ability to heal tissue, restore skin cells, foster phospholipids, and nurture the epithelium.
- Baking soda, sea salt, and magnesium are soothing as mouth rinses and effective as toothpastes due to their alkalinizing-exfoliating action that gently removes plaque. Healthy saliva, a sea of saline alkalinity, contains chemicals and enzymes that exist solely to take care of the teeth. If saliva is too acidic, it dissolves the enamel on your teeth and creates an environment that supports bacteria. With decay, saliva jumps into action to coat the tooth with its beautiful healing fluid. The quality and quantity of saliva also hinge on hydration, so drink up! Paul H. Keyes, DDS and clinical investigator at the National Institute of Dental Research, advised regular brushing with baking soda as it prevents all destructive periodontal disease. It is also significantly less abrasive than the cleaning agents of chalk and silica that are used in many commercial toothpastes.
- Mouth Swishing or “oil pulling” is an ancient Ayurvedic medicinal practice used to detoxify the mouth, teeth, gums, and the entire oral cavity. A small number of studies have been conducted on oil swishing and its impact on halitosis and oral health and have found that oil swishing may eliminate the bacteria that cause oral issues. It is best to oil swish first thing in the morning before you eat or drink. Measure about twenty drops of coconut or MCT oil and two drops of an essential oil (such as Seabuckthorn, rose otto, frankincense, or myrrh, as mentioned above), swish in your mouth for up to fifteen minutes, then spit it in a trash can to prevent the oil from clogging your pipes. Check out Ben's Weekly Roundup post here for a convenient way to make your own “oil-pulling molds.”
- Create strong, healthy dentin, and simultaneously whiten your teeth from within! Tooth enamel is actually transparent, and gray, glassy teeth denote a deficiency in the body of vitamins D3 and K2. These fat-soluble vitamins nourish the dentin, creating shiny, white teeth. Polish off plaque that can get stained by food pigments with one-half teaspoon of 3% food-grade hydrogen peroxide mixed with a teaspoon of baking soda on a dry electric toothbrush once or twice a month.
With the depletion of microbial diversity, you need to build your oral bacterial bank account and SEED it with investments of diverse flora.
- Probiotics act as microbial multipliers. A probiotic-dairy combination was found to reduce the cavity- and periodontal-disease-causing bacteria in the mouth. Providing Lactobacillus reuteri to children from the last trimester through the first birthday has been found to reduce cavities at nine years old. Ben has a great recipe here for making your own L. reuteri coconut yogurt.
- Successful experiments at some dental practices have applied a mixture of probiotics after scaling and root planing called Guided Pocket Recolonization. This can be safely and simply carried out at home with a blunt-tipped syringe filled with a mix of probiotics and a carrier oil, such as MCT.
You can easily make your own oral hygiene products at home that contain a lot of the ingredients I just went over. Below, you'll find recipes for an alkalinizing toothpaste, a potent tooth serum, and a minty, cleansing mouthwash.
Alkalinizing Toothpaste
Ingredients:
- 30 ml Coconut Oil
- 20 ml Baking Soda
- 20 drops Peppermint
- 10 drops Frankincense
- 10 drops Sweet Thyme
Directions: Liquefy coconut oil in a double boiler and add in the other ingredients. Mix together, pour into jars (a different jar for each person in the family), and pop in the fridge to solidify. Once solidified, it can be kept out of the fridge. For an upgrade, infuse the coconut oil with spilanthes (as Ben suggests here), 5ml of activated charcoal, or 6 capsules powdered BPC 157 peptide. To find a doctor in your area who can help you with peptides, visit the International Peptide Society here.
Tooth Serum
Ingredients:
- 20 ml MCT Oil
- 5 ml Frankincense
- 5 ml Peppermint
- 1 ml Sweet Thyme
- 3 drops Oregano
Directions: Mix all ingredients in a shaker bottle. This concentrated chrism is to be used sparingly by the drop to deeply clean between teeth with floss, in a blunt-tipped syringe for cleaning the gum line, or dabbed on cankers or massaged onto gums for extra care. This mix is therapeutically concentrated, so do a patch test before using. For an upgrade, add 3ml Carbon 60.
Mouthwash
Ingredients:
- 10 ml Sea Salt or Baking Soda
- 500 ml Water
- 2 drops Frankincense
- 2 drops Peppermint
Directions: Dissolve salt (you want it to taste as salty as the ocean) or baking soda in warm water. Add in frankincense and peppermint to boost botanical-biotic action. Shake before use.
If you're not the type to dabble in concocting your own products at home, try Happy Gums Clay Toothpaste, Frankincense Fresh Toothpaste, Ozonated Happy Gum Gel, or Happy Gum Drops + Oil Swishing Serum from my company, Living Libations. You can save 15% sitewide when you use code BEN at checkout.
Preparing for a Dental Appointment
Before you go to the dentist, there are steps you can take in order to prepare your mouth, health, and immune system for this type of intervention.
Depending on your overall oral health or what the dentist will be doing, preparing with the following steps for 3 weeks to 3 months prior to your appointment is key.
Preparing for an appointment may seem over the top, but it is important because, after a deep scaling, oral bacteria are dislodged and flow into your bloodstream, challenging your immune system. Your body responds to this perceived attack by releasing white blood cells to combat the invading microbes, and one of the results is systemic inflammation. This is why donating blood is not allowed for 48 hours after a dental cleaning (because your blood is likely to be full of bacteria).
Begin with the classic immune boosters: Vitamin D from sunshine, iodine, NAC, and glutathione. Also add 1,000 to 2,000 mg per day of vitamin C, depending on your health and bowel tolerance. If you are going to the dentist for more serious work than a cleaning, be advised that taking vitamin C orally reduces the numbing effect of Novocain and anesthetics.
In addition, certain peptides offer precise and practical options for optimal periodontal care. Peptides are naturally occurring regulatory signaling molecules that promote your body’s own healing system. There is a trifecta of peptides that I find to be foundational to all aspects of oral care: thymosin α-1, BPC-157, and thymosin β4.
You can use these three peptides subcutaneously in the months leading up to your appointment and then focus-dose before and after appointments, deep cleanings, dental surgeries, and extractions.
- Thymosin α-1 is the immune superhero and is great for pre- and post-dental visits, extractions, cavitation clean-ups, and minor procedures. Thymosin α-1 modulates the immune system by enhancing T-cell function (T-cells are like tiny immunity soldiers that destroy invaders) and by regaining control of cytokines that have “stormed” the body in lieu of boosting immunity.
- BPC-157 BPC-157 seals and heals tissues, gums, and guts. BPC-157 is a complex composition of 15 amino acids found in human gastric juice. It plays a significant role in healing various wounds, and researchers think it may help cure periodontitis. When it was administered to rats with periodontitis, their oral health improved enough to have scientists conclude that, “BPC 157 may represent a new peptide candidate in the treatment of periodontal disease.” It works on multiple pathways in the nucleus of the cell directing the silencing of genes that continue inflammation and promoting the genes that direct blood vessel, connective tissue, fascia, and nerve repair. Leading-edge biological dentists are having success with this very specific, revolutionary peptide protocol with BPC-157 for receding gums. For educational purposes, here is the protocol:
- Dilute BPC-157 (5mg vial of peptide powder) with 1ml NaCl 0.9 (do not dilute with regular bacteriostatic water as that is too painful for gum injections). Note: NaCI will cause a suspension effect and you will see suspensions of particles with this reconstitution.
- Apply a drop of organic peppermint essential oil to the gum/injection site to clean and provide a subtle anesthetization.
- Inject 0.25 ml in the receding gum area (4 injections total: two in upper gum tissues, two in the low area) using smaller dental needles.
- Repeat protocol in 3 weeks.
- Monitor. Repeat a third time if needed.
- Measure gum pockets before and after.
- Effect may be visible in 10 days.
- BPC is also available in powder form (which is rare for a peptide), and this powder can be added to baking soda to make pastes (see below) and tooth-masks. It is also awesome added to oil pulling.
- Thymosin β4 occurs naturally in the human body as an all-around repair molecule, especially soft tissue repair. It is a hormone secreted from the thymus that calms inflammation, stimulates the production of T-cells, and is released by platelets at the site of an injury to trigger a cascade of healing activities. Thymosin also assists in the development of B cells to plasma cells to produce antibodies. It accelerates skin healing in preclinical animal models and in patients.
Before beginning any peptide regimen, inform your dentist. Dentists can reach out to the International Peptide Society for more information.
Summary
When you multiply your mouth’s microbiome, activate your invisible toothbrush by eliminating what hinders the innate functioning of your body, and avoid (or take steps to correct) some of the pitfalls of modern dentistry, the external maintenance of brushing and flossing becomes effortless.
Remember, your teeth are alive and will respond to your efforts! The current condition of your mouth can evolve—enamel can be restored, dentine can be reactivated, saliva can remineralize, and gums can be rejuvenated.
The first proactive step you can take is to begin engaging in proper care of your glorious, bacteria-filled mouth by incorporating the practices highlighted in this article. Next, find a biological dentist to work with. Here is a handy list of questions to ask a dentist before you decide to work with them, and here are some resources for finding a biological dentist in your area:
- International Academy of Oral Medicine & Toxicology
- International Academy of Ceramic Implantology
- International Society of Metal-Free Implantology
For more on natural oral health solutions and biological dentistry, read Ben's article “The Hidden Health Hazards In Your Teeth & What You Can Do About It: Biohacking Your Mouth With Biological Dentistry.” and listen to his podcast “It’s All In Your Mouth: How Your Teeth Are Impacting Your Immune System, Sleep, Performance, Inflammation & Much More (& What You Can Do About It With Holistic Dentistry) with holistic dentist Dr. Dominik Nischwitz. You could also check out my books Renegade Beauty: Reveal and Revive Your Natural Radiance–Beauty Secrets, Solutions, and Preparations and Holistic Dental Care: The Complete Guide to Healthy Teeth and Gums
Now, I'd like to hear from you. Have you made the switch to natural oral care products, or from a conventional to a biological, or holistic, dentist? Leave your thoughts, comments, and questions below and I'll respond.













Very informative! Thanks for sharing this. I agree that we should always choose the products that we use for our body. Natural products are the best!
Hi! I was wondering if there were any alternatives to the coconut oil in your toothpaste? My man really likes your advice and would love to make it for him but he’s allergic to coconut :)
Thank you!
Whan an aaaawesome article!!! OMG, thank you so much for that!! That’s so helpful and clarifying!!
In my country, there aren’t really good options of commercial toothpastes, so I’ll be making my own right away!
So glad this was helpful to you Evandro! Please post an update on how it works out for you!
I could not tolerate the Multiple Sclerosis medications for long. I started on MS Herbal Treatment from VHC, the herbal treatment immensely helped my Multiple Sclerosis condition, i had a significant recovery with this natural treatment. Go to vinehealthcenter. c o m…..
An MRI scan in August of 2014 verified that I had Multiple Sclerosis. I was on Capaxone for months, i was extremely weak, i was barely able to walk. A family friend told us about Mayaka Natural Clinic and their successful MS Herbal treatments, we visited their website w w w. mayakanaturalclinic. c o m and ordered their ms herbal treatment, i am happy to report this treatment effectively reversed my Multiple Sclerosis and symptoms. The treatment reversed my balance issues. I am back on my feet again. My activity level is really up.
Hi,
thanks for an interesting article. I just finished dental school and I have to say I find a few of these information here strange.
1) yes amalgam is toxic but there is a big unknown about the composite materials that are used instead of AMG. There are about 40-60 % free monomers that are not converted into polymers chain. that means that they can go to the bloodstream and we do not have long term studies for these plastic components in our body. At our university there was a big concern about this. (amalgam should be at least stable in its solid state and there should be risk only when a dentist heat it with the drilling)
2) if you extract the tooth that was treated with root canal filling and you put implants instead of it you will never have the same quality. the main problem is that you will lose the colagen attachment around the tooth and more that half of the implants will create peri-implantitis. Your tooth (even endodontically treated treated) has natural barier agains bacteria from the gingiva epitel. with implants you have free way for bacteria into bloodstream soon (and bacteria can couse chronic imflammation anywhere in the body).
I wanna treat my patients the best I can but the truth is there is no treatment without any harm. the only way is prevention.
take care :)
Natálie,
Strange? Listen to the Dr’s that he interviews so they can break down the facts for you.
https://bengreenfieldfitness.com/podcast/biohacking-podcasts/what-is-cyto-detox/
How can you say amalgam is toxic “BUT”?! This is your body and health! No room for buts! And it’s not just toxic, it’s an extremely dangerous neurotoxin that stores itself in your pituitary gland for years, possibly your entire lifetime. Whether it’s an acute exposure or it slowly leaches itself into your body is irrelevant. The danger of putting heavy metals in the body and has been known for 1000’s of years. Are we still drinking wine out of led pots? Using mercury to make hats? Putting led in paint? Mercury in contact solution? Dental mercury has been used for 150 years! I just had my patellar grafted and used it to replace my ACL. Would I trust anyone to do that 150 years ago?! That’s the beauty of health care, we progress and make advancements with new facts and data. The fact that a 150 year old medical practice is still being used today as if it is safe is not only strange but disturbing.
And then you go on to say “should be stable”. It’s either stable or its not. And let’s just be honest here, we all know it’s not. Listen to Dr. Pompa explain this. If you went to a university and studied dentistry in a 1st world country where they had banned the use of amalgam in dentistry would they still teach you the same information? So the treatment of a cavity is mercury and the harm is a life of undiagnosable disease and health complications? but the big concern at dental school is polymers…
We live in what I like to call the mad hatter era. Boomers and gen x’ers have mouths full of metal and there’s no convincing them it’s detrimental to their health. Now, they’re passing down 150 year old practices to up and coming dentists and doctors. So sadly, the misinformation they preach could be passed down as safe facts for generations. We need to end this.
Let’s face it. Mercury is used as a filling because it’s the cheap and easy route. It’s a malleable substance and someone thought 150 years ago would be a safe and effective treatment in dentistry. Now, in 2020, we know, through facts, data, and the use of instruments to measure it that amalgam fillings are anything but safe. Please don’t finish dental school and continue this practice plaguing yet another generation of young adults and children with mercury tox before they can even think for themselves..
Ben Wozniak
I’m a Dental Hygienist. This article is so disturbing on so many levels. As a seasoned hygienist, misinformation of this nature, is my biggest frustration.
What first caught my attention was the mislabeled parts of the tooth.😬 I had to quit reading when I reached the part about making an incision where the wisdom tooth was removed and removing the decay from the bone! Oh, my.
There are no biological dentists in my area, do you recommend someone who gives online consultations? I believe my issue is mainly a nutritional deficiency and i’d like to heal some cavities.
Hi Maria! Thank you for your message. We recommend Dr Judene Benoit who offers virtual video consultations.
Thank you so much Nadine! <3
Hey Maria,
I’m a biological dentist and yes, I do give online consultations! I can help you find someone in your area and answer any questions you have.
You can DM me @thedentistnextdoor
Blessings,
Jacquelyn Freeman, DDS
Thank you Jacquelyn! I’ll be emailing you. :)
I traveled from my home in Montana to Tijuana and had four mercury amalgam removals removed. There are a handful of dentists down there who are recommended by the IAOMT for safe amalgam removal. Plane tickets to San Diego are very cheap and the cost of care is so much cheaper down there that it was less than half what I would pay up here. The care I received was on par with any I’ve had in the states without even considering the special protocols they utilized. Just something to look into for those of us without insurance…
any recommendations? I’m in LA and the girl I’m dating currently has a mouth full of amalgams at 25! She thought she would get them taken out in China but I think she may be better off in Tijuana which sounds like a fun trip from LA anyway :)
Mitch,
Any dentists in TJ you can recommend? I live in SD and need to find a good dentist. I’ve often heard going to TJ was a great inexpensive
Option.
What a pertinent time for this to come up
In my inbox. It’s 4:00am in the UK and I’m awake having had a horizontally growing wisdom tooth and the tooth next to it that was severely decayed extracted yesterday as I was getting repeated infections and problems 🤦🏼♀️
I looked into holistic dentistry to have amalgam fillings replaced and generally check me over as I also have receding gum issues. The problem is that it was going to cost about £10,000 to have everting I needed done – the fillings and some crown replacements….he said that my root canals showed no signs of infection issues and could be left as they are. Sadly that’s makes it too expensive to do.
Whilst he is not ‘Mercury free’ my normal dentist was not against doing the filling removals/replacement procedures and would use a dam to help prevent any mercury ingestion. This way I could afford it. Hopefully this and adopting more of the techniques mentioned here is the right way forward 🤞🏻
The good news is that anyone can elevate their oral ecology with these tips. We do recommend consulting with several biological dentists to find one that you trust.
This is a handy link when consulting with a new dentist: https://livinglibations.com/pages/what-to-ask-a-prospective-dentists
Does anyone have thoughts on Xylitol?
Hi Brad! Heralded as an ally in the battle against tooth decay and diabetes, xylitol is another sweetener to enter the market with a great deal of hype.
Studies funded about Xylitol inhibiting cavities have been funded by the Xylitol industry.
There are dubious claims that xylitol prevents cavities but the results of a recent two-year trial found no difference in cavities between those who chewed xylitol-containing gum and those who did not.
In an earlier study, researchers concluded that “overall, consumption of xylitol-containing snacks and candy did not reduce S. mutans levels.” (J Am Dental Assoc, 2002;133(4):435-441.)
In one 2006 article in the Journal of the American Dental Association, “Xylitol-sweetened gum was noncariogenic in all of the protocols tested. Some studies claimed that xylitol-sweetened gum had an anticariogenic effect, though these claims need further study.” What this means is that xylitol gum did not promote cavities, probably because of its lower alteration of blood sugar versus regular sugars. However, the anticariogenic effect needs further study, and the idea that xylitol actually inhibits cavities remains to be proven according to this author.
In a long term toxicology study on rats “it was concluded that xylitol caused a significant increase in the incidence of adrenal medullary hyperplasia in male and female rats in all dose levels tested (5%, 10% and 20%).” (Russfield, A.D. (1981) Two-year feeding study of xylitol, sorbitol and sucrose in Charles River (UK) rats: Adrenal Medulla. Unpublished report.)
Thanks Nadine! I was not aware that the 2013 study that found no significant benefit..
I looked up that 2013 study and at the same time found a 2017 study claiming a benefit.
To the extent anyone is interested, I posted links to both studies below.
Now you have me wondering as to whether there are also mixed findings with cranberry juice.
2013 Xylitol Study
https://pubmed.ncbi.nlm.nih.gov/23283923/
2017 Xylitol Study (No apparent funding by the Xylitol industry)
https://link.springer.com/article/10.1007/s00784-017-2075-5
What happens if you get veneers? What happens to the dental lymph? Do the teeth still sweat? Do you still have the same bacteria in your mouth?
The research on how dentinal lymph flow is affected by dental substrates (such as veneers), and tooth surface prep work is still in its infancy, and researchers are not yet ready to make definitive claims. So, we can only share with you what dental research believes to be true right now.
There are many types of veneers, and each one requires a different type of tooth prep and adhesion: some veneers are glued directly on top of the tooth as it is, some require grinding down the enamel, and some etch all the way into the dentin. Unless the tooth is dead or root canalled (which we don’t recommend), there will be health-giving fluid flowing into the tooth and keeping it alive. Dentinal fluid, of course, cannot flow up and out through artificial materials, such as porcelain, resin, and adhesive. The dentinal fluid flow stops where your natural tooth stops. What happens to the microbeads of “sweat” under the veneer is yet a mystery—we haven’t found any research that has looked into this—though it is most likely reabsorbed by the remaining natural tooth surface.
Research has indicated that bacteria have a different relationship with veneers (as well as fillings and crowns), than with natural teeth, yet research is still scarce. We do know that bacteria can form biofilm on dental materials (veneers), and the materials’ surface roughness or smoothness, as well as their chemical composition, probably affect how and where biofilm forms. We also know that biofilm degrades dental materials, which roughen the surface and further enhances biofilm development. This could encourage periodontal issues. So, if you have veneers, it is really important to brush, floss, and swish and take extra care around the gum line to keep biofilm at bay. The good news is that antimicrobial dental materials that hold up better under bacterial challenges are being researched and may be available soon.
You should ABSOLUTELY include Dr. Ellie Phillips in the mix. She’s been advocating for the value of saliva to our overall health for some time, now, and helping people feel empowered to look after their oral microbiome themselves.
I have been practicing periodontics for 44 years and have been incorporating anti-inflammatory nutrition and a paleo lifestyle with my periodontal therapy. Recently, I recently published a mini-eBook titled, “Is Your Gut Killing You?”
My clinical experience and research show that a dysbiotic gut creates increased intestinal permeability and a compromised immune system. Various factors will cause a change in the healthy balance of microbes in the gut. But once a pathogenic change occurs, the immune system becomes compromised, which creates systemic inflammation and affects the oral microbiome negatively. There is significant crosstalk between the gut and the mouth. Poor food choices then will cause potential pathogenic bacteria in the mouth to overgrow and begin the progression of periodontal disease and dental decay.
To return the mouth to health, gut dysbiosis must be treated appropriately and the oral microbiome must be brought back into a state of balance.
I would love to have a conversation about how to treat the gut and the mouth to improve overall health and recreate a robust immune system.
Yes Ben please look into making this a reality!
Dr. Al–loved your conversation with Paul Saladino. Absolutely fascinating. And congratulations on recovering your health!
Recently Mehran Tavakoli Keshe did gave a hint on how reverse cavities in teeth in his Knowledge Seeker Workshop Series
Swirl regularily with “liquid Plasma” of CO2- & Zn-GaNS for satisfying the Nervous System & Emotions
https://en.kfwiki.org/wiki/Category:GANS
Chew a piece of cheese (form goat or A2 cow milk) after brushing your teeth.
Hello,
I am looking to improve the remaining of my teeth. I have many big fillings and some close to the nerve.
Do you have any links to the trifecta peptides that can be purchased in Canada?
Ben has awesome resources for peptides that ship to Canada. He has also interviewed Jean Francois Tremblay on his podcast and his company, CanLab, is in Canada.