December 16, 2013
Now I don't have anything against big booties, but when it comes to fitting into your skinny jeans, sometimes a big butt just ain't your friend. What most people don't realize is that before you get that big butt, you've probably developed a broken gut. And I'm not talking about your muffin tops or your waistline fat. I'm talking about what's inside your gut.
Particularly, hormone imbalances in your gut.
So…do you have hormone imbalances?
Maybe you have no clue. That's OK. Let's simply find out with a few more questions…
Do you have trouble falling asleep at night?
Do you spend more time daydreaming about Duck Dynasty than you do focusing on your work?
Do you get sick if anyone sneezes within a one mile radius?
Do you snap when you're stuck in traffic, the internet is slow, or someone smiles wrong at you?
Do you have trouble recovering from that workout you did…a week ago?
If you answered yes to any of those questions, you probably have a bit of hormonal funkiness going on. Today, in this guest post from Dr. Tim Jackson, who is the mastermind behind the “Heal Your Hormones Bootcamp” you're going to learn why (among other things) hormone issues can even cause some serious problems with fat loss, and what you can do about it.
Where Do Hormone Imbalances Come From?
We now live in a world where hormone imbalances run rampant in individuals as young as their early 20’s. While everyone realizes the decline of sex hormones and possibly thyroid hormones as they enter their 40s and 50s, few people understand the ubiquitous nature of endocrine disruption in people as young as 20 and 30 years old.
The decreased sex hormone production that happens in older individuals is well documented and is due in part to decreased output from the ovaries and testes. But what accounts for the relatively recent (within the past 20-30 years) decline in sex and other hormones in increasingly younger populations? The problem is multifaceted and contains several layers.
For one, we are essentially cave men and women walking around with electronic devices: in other words, we are not adequately equipped to deal with the thousands of endocrine-disrupting chemicals like BPAs, BHC, PCBs, etc. that are rampant in our food supply, air, and water. Both external stress (such as relationship or financial stress) and internal stress (like viruses, heavy metals and blood sugar swings) contribute to hormonal disruptions. Dietary contaminants, such as GMOs, antibiotics, and synthetic chemicals, also contribute to hormonal disturbances.
But one lesser-known mechanism behind hormonal imbalances is poor digestive health.
How Your Gut Hormones Break
Let’s unravel this digestion thing because it is severely misunderstood – and you cannot have optimal health or even good hormones without good digestion. Every nutrient in the body must pass through the gut. If any type of malabsorption or dysbiosis exists, all of the cells in the body will become deprived of nutrients needed for basic daily functions, like magnesium, zinc, and all of the B vitamins.
Vitamins, minerals and the component parts of fats, proteins and carbohydrates are needed to make your cells run efficiently, particularly the cells of the thyroid, adrenal glands, testes, ovaries, etc.
So…decreased nutrient levels equals impaired hormone production.
You with me so far?
So, what causes this malabsorption or dysbiosis? Malabsorption can be caused from decreased hydrochloric acid (stomach acid) production, insufficient bile salts, or decreased enzyme levels. Dysbiosis occurs when the ratio of good to bad bacteria in the colon is altered, resulting from antibiotics or over-consumption of carbohydrates.
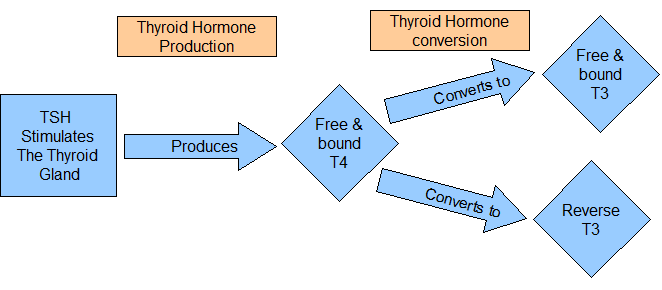
Both these issues can impact your hormones on several levels.
Consider this: roughly 20% of T4 gets converted to T3 (your active, metabolism-boosting thyroid hormone) by good bacteria in the digestive tract. So if a dysbiosis is present, there is an increased likelihood that some of your T4 will not be converted efficiently into T3. Instead, more reverse T3 will be produced, which binds to T3 receptors but does not induce any of the good actions of T3. What a waste.
Secondly, most toxins in the body are conjugated and excreted with bile via bowel movements. An enzyme known as beta-glucuronidase is elevated in people with dysbiosis. This leads to the de-conjugation of estrogen – meaning estrogen is not excreted with other toxins as nature intended. This allows estrogen to re-circulate throughout the body and wreak havoc.
Excessively elevated estrogen is pro-inflammatory and inhibits mitochondrial respiration, leading to decreased energy production and a decrease in overall tissue function. In addition, as an unpleasant double-whammy, elevated estrogen will prevent T4 from converting to T3.
So now you know…
…Gut dysbiosis and impaired liver health→Elevated estrogen→Increased thyroid binding globulin and decreased T4 to T3 conversion→Decreased free T3→Decreased metabolism…
…=Weight gain.
Heard of Leaky Gut?
Another way poor digestive health impacts hormone levels is via added stress to the Phase I and Phase II liver detox pathways. Your liver uses two distinct phases to metabolize toxins, preparing them for exist out of the body. Phase I involves converting fat-soluble toxins into water-soluble substances, with highly reactive substances being created. These substances then enter Phase II detox, which works on neutralizing those reactive compounds.
Any sort of digestive issue, especially elevated levels of gram-negative bacteria like Pseudomonas Aeruginosa, will slow down the normal mechanisms of liver detox. Gram-negative bacteria have lipopolysaccharides, or LPS, as part of their outer wall. These LPS can be released from the bacteria and irritate the mucosal lining of the digestive tract. If this happens enough, the gut barrier is breached (“leaky gut”) and the LPS reach the bloodstream.
This LPS in the bloodstream creates an inflammatory response system-wide and contributes to decreased thyroid receptor sensitivity. In addition, once the liver absorbs the LPS, they slow down Phase I detox.
This is a big issue, because roughly 60% of T4 gets converted to T3 in the liver. The majority of our other hormones are also metabolized in the liver. If the liver pathways are over-burdened with LPS and toxins from the gut, hormone imbalances are inevitable. In addition, elevated levels of LPS can contribute to insulin resistance and the subsequent downstream hormonal alterations.
So now you know…
…Lipopolysaccharides from gut bacteria→ Impaired liver detox pathways→Hormone imbalances….
…=Weight gain.
Where Pregnenolone Fits In
So far, we have discussed thyroid and estrogen levels. Now, it is time to shift gears and give something called pregnenolone a little love.
Pregnenolone, aka ‘the mother hormone’, serves as the steroid precursor to all of our sex hormones, cortisol and mineral corticoids. During times of both internal and external stress, our bodies will sacrifice the production of our sex hormones in favor of more cortisol.
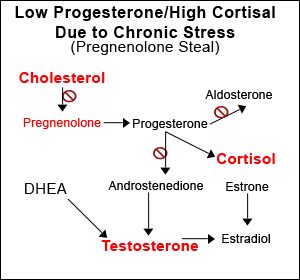
Remember: you can live without estrogen, testosterone, progesterone, etc., but you cannot live without cortisol because it is critical to your day to day existence!
What constitutes a stressor?
In short, anything that creates inflammation in the body. Inflammatory sources will activate the adrenals to produce cortisol, our natural fire retardant. Gut infections (parasites, bacteria, yeast) all count as stressors to the body that will require the production of cortisol at the expense of the sex hormones. One can supplement with adaptogens, exogenous hormones, etc., but until you uncover the source of the stress, it is analogous to pouring water into a leaky bucket.
So the ultimate goal for optimal health and healthy weight loss is to eradicate any source of inflammation in the body.
To add insult to injury, once cortisol elevates past a certain level, it will contribute to a thinning of the mucosal lining in the digestive tract (making it even more ‘leaky’). This allows the passage of microbes and food particles that normally would remain in the GI tract into the blood stream, creating an inflammatory response and a vicious cycle.
In addition to thinning the gut mucosa, high cortisol levels lower secretory IgA, an important component for maintaining gut health and preventing GI infections. This is one of way in which high cortisol suppresses immune performance.
This is also why people who have completely normal guts can go through a period of stress in their life (e.g. death of a loved one, broken relationship, new stressful job or school, etc.) and suddenly have leaky guts, food allergies, skin problems and all sorts of new mysterious illnesses. It's all cortisol-gut related!
Gut, Thyroid & Sex Hormones Are All Connected
Optimal thyroid function is needed for the formation of the gut-associated lymphoid tissue, abbreviated “GALT”. GALT serves as the one of the body’s storage bins for T cells and B cells, two important types of immune cells. In addition, optimal thyroid levels are needed for the production of hydrochloric acid in the stomach. Without sufficient stomach acid, the entire digestive sequencing is disturbed: the release of bile from the gall bladder is decreased, the production of enzymes from the pancreas is decreased, etc. The altered pH status in the respective areas of the digestive tract impacts the microbiome, increasing the likelihood of a bacterial, fungal or parasitic infection.
In addition, sub-optimal thyroid function decreases both liver and gallbladder function. Testosterone also exerts influence on the microbiome of the GI tract. In rodent studies, increasing testosterone increased the level of good bacteria in the gut, possibly explaining why women are at an increased risk of some auto-immune disorders due to their lower levels of testosterone (in addition to the increasingly and disturbingly large number of the male population who now have plummeting testosterone levels).
Begin By Optimizing Digestion
Whether your goal is to play professional sports, lose a few pounds and shed that big butt, or be fully present for your family and friends, optimizing digestion provides the greatest health return on investment.
Things you can do to optimize digestion include:
–balancing stomach acid, which is commonly low (not high as the media would have you believe)…
-ensuring adequate bile and liver health by eating foods similar to those shown on the below image…
-addressing any bacterial, fungal or parasitic infections found via stool testing (e.g. the “GI Effects Chemistries Profile” panel through DirectLabs)
What About Hormone Replacement Therapy?
With integrative medicine and wellness becoming increasingly accepted, hormone replacement clinics are popping up all over the country. Many of these doctors and practitioners are new to the field and have likely only studied hormones alone and not their interactions with the other body systems. So if you opt for this solution – proceed with caution and try the other fixes first!
Even for those who require hormone replacement therapy, repairing your digestion will help you get the most out of your therapy by reducing inflammation and providing the cellular nutrition needed to deliver those hormones to the correct areas in the body.
Lastly, optimizing the GI tract reduces the risks of side effects from hormone replacement therapy- such as developing fat around the chest for men and the development of facial hair for women – by decreasing the workload on the liver, your body’s hormone processing center.
Summary
As you can see, shedding fat is about far more than simply killing time on a treadmill.
It's about getting rid of endocrine disrupting chemicals.
It's about fixing bacterial imbalances in your gut.
It's about decreasing stress.
If you want to shed that big butt, you have to first repair your broken gut. And now you know why, along with where to start. Leave your questions, comments and feedback for Dr. Tim Jackson, the Heal Your Hormones Bootcamp or for Ben Greenfield (editor of this post) below, and we promise to answer!
About the Author
Dr. Tim Jackson, DPT received his undergraduate degree in Health science and chemistry from Wake Forest University in 2003. He completed his Doctorate in Physical Therapy (DPT) from the Medical University of SC in 2009. Realizing that manual therapy and orthopedic care helped only some of his patients, he began studying functional and environmental medicine, as well as digestive health, in an effort to help others achieve wellness.Dr. Tim is educated in nutritional biochemistry, digestive health and its systemic effects, as well as functional endocrinology. He recently completed the Spine portion of the Active Release Technique methodology, a system that addresses musculoskeletal trigger points and helps to expedite the healing process. Currently, Dr. Tim is working on his Functional Diagnostic Nutritionist certification.




Great article, this is EXACTLY what happened to me too! Even after I moved to Paleo, the problem was NOT fixed as it did for most Paleo people. In fact, I was not able to lose weight as other people did on this diet, and when I went too low carb, even more Reverse T3 was produced, so I couldn't lose weight at all, and felt like a zombie. Not only that, but my liver is still fatty, and my triglycerides are off the roof. This is unheard of for 95% of the Paleo dieters. But it's what's going on with me, and after lots of research online, I also arrived at the same conclusions as this article, but this article puts everything in one page. I'm still Paleo, but higher carb, in order to prevent my rT3 from overreacting (I have to stay Paleo forever because of my gluten/food sensitivities). After 2+ years on the diet, I'm still obese. I've only lost 10-15 lbs since then. Honestly, I'm not sure it's easy going away from this vicious cycle. If I eat higher carb, I can function, but I don't lose weight. If I eat less carbs or less calories, I become a zombie due to rT3. Chicken and the egg. Moreover, it's recommended that people with high rT3 to not supplement with synthroids, but try to manage it naturally. Honestly, I don't see how this is possible, my case is a pain in the bum.
Hey Every1FitChick! It's not possible–to my knowledge–to determine how something from the past may be contributing. The key is to find the hormone imbalances and correct them, along with digestive disturbances, liver issues, etc. If cortisol is high, there are plenty of supplements to lower it. But the question remains…why is it high?
Awesome article! Thank you for your diligence in studying and presenting information to people.
I went through some massively stressful situations in the past couple of years and I am wondering if this may have something to do with my seemingly inability of losing weight over the last two years. I have been bringing every possible circumstance into consideration.
So how would I go about finding out if this in fact apart of my issue? Is there a way to "diagnose" this?
Also, what have you found to be the best way to lessen the inflammation caused by cortisol?
Great post Tim! This is complex information made easy. What would you suggest for someone that has DNA mutations and therefore impaired liver detox in BOTH phase 1 and phase 2?
It depends on the SNPs/mutations in Phase I. Many of Phase I SNPs may cause issues with certain medications. Others, such as CYP1B1, 1A1, may cause issues with estrogen metabolism. Things like Calcium d-glucarate can be helpful for that. For SNPs like MTHFR, you need B12 and methyl-folate, or L-5MTHFR.
I do have the CYP1B1. I have tried Calcium d-glucarate, but that increased the mysterious muscle weakness I developed after doing some cleansing. Figure that one out!! I also have CYP2A6 and CYP2C19
I had 95% of my thyroid removed when I was a teenager. I don’t have any real issues with my weight but do find it hard to maintain my energy & stress levels often getting burnt out!
Can you advise on best way to deal with this!
I would consider natural thyroid replacement therapy. Dr. Tim goes into this in the Heal Your Hormones workshop. I've personally used Thyrogold in the past.
Thanks Ben I have ordered some Thyro_gold will give it a try ;)
How do you explain a ton of fluid retention (about 12 lbs) if all hormones are WNL (within normal limits) ? you name a hormone and it's fine :/ cortisol is normal, Thyroid is fine, Estrogen is fine and so on….. Male 40 yrs old. Basic chem panel is fine, melatonin is fine, RBC/WBC fine, BPN is fine, and a million other lab tests – all ok. UGH! I"m confused. I eat a very strict Epi-Paleo (Jack Kruse) diet. Do grounding, mediate daily, CT, and a million other daily tasks to stay healthy. No idea ? :(
A hormone being WNL and being optimal are VERY different! :) You need your labs in front of someone who knows how to properly analyze them. In addition, other factors must be addressed…chronic sub-clinical infections, digestive health through testing, neurotransmitters, etc.
Intersting post. When you talk about LPS and bacteria and estrogens recirculation is that primarily from the large intestine or small?
LPS come from gram-negative bacteria, which are usually in the large intestines. BUT if bacteria move up to the small intestines, then they can inhabit that structure as well. Normally, there should be very little bacteria in the small intestines. The estrogen re-absorption usually comes from an enzyme produced by bad bacteria in the large intestines, or colon.
Thanks once again for a great article. I have been on synthroid for 20 years so am wondering if that has anything to do with my on and off again stomach issues. About one week a month I get bloated and have digestive issues. I also can’t seem to process alcohol and get hungover very easily. Not sure where to start or what test to take but my “gut” feeling is that somethings not right. Thanks for any advice!
It could certainly have something to do with it. I don't like Synthyroid. Many people are poor converters of T4 to T3. You need selenium, iodine, zinc, etc. to convert properly. If estrogen or cortisol is less than optimal, the conversion won't happen efficiently. I prefer Armour and/or Cytomel.