January 9, 2018
Yeah, yeah, I know it's risky to begin a blog post with a big scary phrase, but I'm going to do it anyway – because this phrase is a big elephant in the room that nobody is talking about and that phrase is…
…”glycemic variability.”
In a nutshell, as you can see in the article, “Glycemic Variability: How Do We Measure It and Why Is It Important?“,
Glycemic variability (also known as “GV”) refers to blood glucose oscillations that occur throughout the day, including hypoglycemic periods and postprandial (after a meal) increases, as well as blood glucose fluctuations that occur at the same time on different days. According to the article I referred to above “the broad definition of GV considers the intraday glycemic excursions, including episodes of hyperglycemia and hypoglycemia”.
Now, if you find white lab coats sexy, science makes you salivate, and you know your biochemistry cycles back-and-forth, you may want to get into the nitty-gritty science of glycemic variability in this fantastic podcast by my friends from NourishBalanceThrive.
But in plain speak, glycemic variability basically refers to how much your blood sugar bounces around at any given point in your life. And when it comes to your health, it is, in my opinion, a more important variable to consider than cholesterol, vitamin D, minerals, telomere length, cortisol, testosterone or just about any biomarker one could ever measure (except, perhaps, inflammation, which I would rank right up there with glycemic variability).
This is why, in the food presentation I gave last month in New York City, entitled “A Biohacking Adventure: 7 Culinary Tactics For Enhancing Health & Longevity”, I began by tackling the concept of glycemic variability, and discussing a host of tactics to keeping blood sugar fluctuations at bay, including chewing your food 25-40 times, carb backloading, the pre-meal use of digestifs and bitters, two teaspoons of ceylon cinnamon each day, berberine, apple cider vinegar, fish oil, pre and/or post-meal physical activity and much more.
But perhaps you couldn't make it to New York City. So in today’s article, I'm going to hone in on this most prevalent of conditions that threaten longevity today, and fill you in on many of the tactics I covered in my presentation at Bouley's, along with a few extra goodies for you.
Why What You Are About To Read Is So Darn Important.
This is, in my opinion, one of the biggest leading causes of chronic disease and aging in humans. As a matter of fact, my brilliant friend, surgeon and longevity physician Dr. Peter Attia has said in the past in this fascinating interview on the eight keys to longevity that “…the name of the game is glucose disposal. Can you maintain a low average level of glucose and a low variance of glucose and a low area under the curve of insulin?”
In other words, despite any other anti-aging measures you pursue, if fluctuations in blood sugar or high blood sugar overall are left untreated, it can lead to a life cut short, depriving you of the long years that you could have with your family and friends. Sadly, just recently a new CDC report revealed that more than 100 million Americans have diabetes or “pre”-diabetes (basically pre-diabetes is chronically elevated blood sugar).
Since my own personal genetic testing has revealed that I have a higher than normal risk for Type 2 diabetes (there are specific genetic variations associated with diabetes that you can check out here), hacking blood sugar levels to get them lower is a topic near and dear to my heart. This should also be a very important topic for you to educate yourself on, since not only are Type 2 diabetes rates rising, both in the United States and globally (even among athletes and so-called “healthy” people), but so are a host of other chronic disease, neural degradation and weight issues directly related to high blood sugar. Characterized by insulin resistance and chronic high blood sugar levels (hyperglycemia), type 2 diabetes can lead to both brain and metabolic dysfunction, and is also a significant risk factor for cardiovascular disease (especially if you’re experimenting with something like a high-fat diet, since sugars can easily adhere to cholesterol particles from that cup of fatty coffee you’re drinking and make a high-fat, low-carb diet highly atherosclerotic).
When blood sugar is chronically elevated, the insulin released by the pancreas becomes progressively less effective in bringing those blood sugar levels down, and ultimately, pancreatic tissues begin to suffer damage (although some evidence shows this pancreatic damage can be reversed with specific lifestyle and food strategies). Although blood sugar can slightly rise in response to factors such as stress, hard exercise, or long periods of sedentary time, blood sugar typically rises most significantly after a meal, and studies show that these post-meal or “post-prandial” hyperglycemic spikes are the most likely to lead to vascular complications, even when compared to elevated fasting glucose levels.
When it comes to controlling high blood sugar, your body has two choices: get rid of the blood sugar as potential energy via uptake into muscles, or store the blood sugar in fat tissue. So in this article, you’re going to get five ways to control your blood sugar without it simply getting partitioned into fat tissue, you’re going to learn how to get rid of stubborn carbohydrate related body fat (and even reduce your risk of diabetes based on the latest medical research on exercise and blood sugar), and you’re also going to learn why sugar in your food isn’t as big a deal as you’ve probably been led to believe that it is.
Oh yeah, and one quick thing before we dive in…
…I am not a doctor and this is not to be taken, interpreted or construed as medical advice. Please talk with a licensed medical professional about this. These are just my own personal thoughts and not a prescription or a diagnosis or any form of health care whatsoever.
News Flash: Sugar In Your Food Isn’t Always Bad
Prepare to be shocked. Ready? Okay, here we go…sugar is probably not as bad as you may like to believe. Yes, you heard me right.
These days, it seems that sugar is one of the most demonized substances on the face of the planet, and I have been flabbergasted at the number of people who will look at the label of, say, an extremely healthy protein powder or adaptogenic herb complex or kombucha bottle and completely flip out over the five to ten grams of sugar or fructose or dextrose or maltodextrin that they see on the label of the package. This practice becomes even more shocking when you look at the level of physical activity in these folks: Ironman triathletes, Spartan athletes, CrossFitters, and people for whom this amount of sugar is truly a speedbump when it comes to any amount of metabolic damage.
This would fall into the category of what I have, on a previous podcast, deemed as “orthorexia“, an unhealthy obsession with analyzing every tiny ingredient on a food label and flipping out if there's even a semblance of something that might make you fat or bump up your blood sugar or be a “toxin”.
And yet you hear the same things over and over again, often from extremely active, insulin-sensitive people:
“Sugar is toxic!”
“Any sugar gets turned into fat in the liver!”
“Sugar oxidizes cholesterol, no matter what!”
“Sugar causes massive insulin spikes that make you fat!”
“Sugar rips you out of ketosis and fat-burning mode!”
Whenever I hear such extreme statements made about sugar, I get just a little bit annoyed, and you're about to discover why.
What Is Sugar?
Let's first look at what sugar really is.
In nutrition science, there are three forms of sugar: monosaccharides, oligosaccharides and polysaccharides.
Monosaccharides are often called simple sugars because they have a very simple structure (mono means one and saccharide means sugar). Monosaccharides include glucose, fructose, and galactose.
Glucose is a type of sugar that is most commonly known as blood sugar and is found in your blood and produced from the food you eat. Most food-based carbohydrates contain glucose, either as the only form of sugar or combined with fructose and galactose. So when you hear people talk about blood sugar levels, they’re referring to the amount of the monosaccharide glucose in the blood.
Then there's fructose. Fructose is a sugar naturally found in fruit, and also in processed products such as sucrose (table sugar) and high-fructose corn syrup (HFCS), both of which are about 50% fructose and 50% glucose. Fructose is basically converted into glucose by your liver and then released into the blood as blood sugar. Finally, galactose is a type of sugar found in dairy products and it’s metabolized similarly to fructose.
Okay, let's move on to all oligosaccharides. Oligosaccharides are molecules that contain several monosaccharides linked together in a chain. These sugars are one of the components of fiber found in plants, and your body is able to partially break down some of these oligosaccharides into glucose. Vegetables (shocker!) even have sugar in the form of fructo-oligosaccharides, which are short chains of fructose molecules. These chains are broken and the individual fructose molecules are then converted into glucose. Raffinose, for example, is a common form of oligosaccharide and is comprised of a chain of galactose, glucose, and fructose, and is found in healthy foods like beans, cabbage, Brussels sprouts, broccoli, asparagus, and natural, whole grains.
Then there are polysaccharides, which are long chains of monosaccharides, with ten or more monosaccharide units. Starch from plants and cellulose, a natural fiber found in many plants, are two examples of polysaccharide “sugars” (so toxic, eh?). Your body is able to break starches down into glucose, but not cellulose, because it passes through your digestive system intact…
…but every single sugar you just discovered, whether it's from vegetables, whole grains, or a can of soda, mostly winds up as glucose. As a matter of fact, every shred of carbohydrate you eat is either metabolized into glucose or is left undigested as dietary fiber, and your body truly can’t tell the difference between the sugar found in fruit, honey or milk, or a candy bar. They’re all broken down into monosaccharides, which are then turned into glucose, which are then transported to your brain, muscles, and organs.
Now don't get me wrong: I'm not saying that you should forgo the salad for a cup of ice cream or the bowl of broccoli for a Snickers bar because it all winds up with the same metabolic fate, but I do want you to understand that you're probably eating “sugar” no matter whether you realize it or not.
When Sugar Is Bad
So, when is the intake of sugar actually a problem? To answer that question let's turn to this whole “sugar is toxic” argument.
On May 26, 2009, Robert Lustig gave a lecture called “Sugar: The Bitter Truth,” which was posted on YouTube. The video has been viewed over 800,000 times, gets new viewers at a rate of about 50,000 per month, and is basically a 90-minute discussion of the subtle nuances of fructose biochemistry and human physiology.
In the video, Lustig presents the argument that sugar is a “toxin” or a “poison,” referring not only to the white granulated sugar that we put in coffee and sprinkle on cereal (sucrose) but also high-fructose corn syrup (HFCS), which Lustig calls “the most demonized additive known to man.”
He claims that sugar is not just an empty calorie, and that “It’s not about the calories…it has nothing to do with the calories. It’s a poison by itself.”
But in a 2010 review of the science of sugar, entitled “Misconceptions about fructose-containing sugars and their role in the obesity epidemic”, Luc Tappy, a researcher at the University of Lausanne in Switzerland who is considered by biochemists who study fructose to be the world’s foremost authority on the subject, said there is “not the single hint” that HFCS was more deleterious than other sources of sugar. Here’s what Tappy has to say:
“A causal role of fructose intake in the etiology of the global obesity epidemic has been proposed in recent years. This proposition, however, rests on controversial interpretations of two distinct lines of research. On one hand, in mechanistic intervention studies, detrimental metabolic effects have been observed after excessive isolated fructose intakes in animals and human subjects. On the other hand, food disappearance data indicate that fructose consumption from added sugars has increased over the past decades and paralleled the increase in obesity. Both lines of research are presently insufficient to demonstrate a causal role of fructose in metabolic diseases, however. Most mechanistic intervention studies were performed on subjects fed large amounts of pure fructose, while fructose is ordinarily ingested together with glucose. The use of food disappearance data does not accurately reflect food consumption, and hence cannot be used as evidence of a causal link between fructose intake and obesity. Based on a thorough review of the literature, we demonstrate that fructose, as commonly consumed in mixed carbohydrate sources, does not exert specific metabolic effects that can account for an increase in body weight. Consequently, public health recommendations and policies aiming at reducing fructose consumption only, without additional diet and lifestyle targets, would be disputable and impractical. Although the available evidence indicates that the consumption of sugar-sweetened beverages is associated with body-weight gain, and it may be that fructose is among the main constituents of these beverages, energy overconsumption is much more important to consider in terms of the obesity epidemic.”
In a nutshell, what research actually shows is that sugar-sweetened compounds are bad for us not because there’s anything particularly toxic about the sugar they contain but just because people consume…
…too much sugar.
The list of research backing up this idea that sugar is not the issue but that overeating sugar is the issue goes on and on.
One extensive review of HFCS literature that says:
“Sucrose, HFCS, invert sugar, honey and many fruits and juices deliver the same sugars in the same ratios to the same tissues within the same time frame to the same metabolic pathways. Thus…it makes essentially no metabolic difference which one is used.”
Here’s one from an Another HFCS literature review says:
“Based on the currently available evidence, the expert panel concluded that HFCS does not appear to contribute to overweight and obesity any differently than do other energy sources.”
And another literature review says:
“The data presented indicated that HFCS is very similar to sucrose, being about 55% fructose and 45% glucose, and thus, not surprisingly, few metabolic differences were found comparing HFCS and sucrose. That said, HFCS does contribute to added sugars and calories, and those concerned with managing their weight should be concerned about calories from beverages and other foods, regardless of HFCS content.”
The bottom line is that fructose is just another simple sugar and can only harm you when you over-consume it. And, as you learned earlier, sucrose occurs in completely natural foods like pineapples, sweet potatoes, beets, sugar cane, walnuts, pecans, and cashews.
Here’s another shocker. In this study, researchers from The Sugar Bureau in the UK found that increased sugar intake was associated with leanness, not obesity, and concluded that there simply wasn’t enough evidence to warrant a quantitative guideline for sugar consumption. Another study, at the University of Hawaii, which is an extensive review of sugar-related literature, quoted:
“It is important to state at the outset that there is no direct connection between added sugars intake and obesity unless excessive consumption of sugar-containing beverages and foods leads to energy imbalance and the resultant weight gain.”
With all of that being said, here's what happens inside your body when you ingest sugar.
How Sugar Gets Into Muscles
Before discovering how certain strategies can lower or stabilize your blood sugar, it’s important to understand how sugar gets transported into muscle in the first place (you can dig into the science of everything you’re about to read in this research article).
The entry of glucose into muscle cells is achieved primarily via what is called a “carrier-mediated system” which consists of small protein transport molecules. One of these transport molecules called “GLUT-1”, is normally found in the sarcolemmal membrane (a sheath that surrounds your muscle fibers) and is thought to be involved in glucose transport under basic resting, non-active conditions.
When the hormone insulin gets released by your pancreas, which is something that can happen after a large meal of protein (yep, whey protein can spike blood sugar and insulin higher than a candy bar) or carbohydrates, glucose transport can be accelerated even more because insulin upregulates the activity and the number of yet another sugar transporter called “GLUT-4”, which, just like GLUT-1, is found in skeletal muscle, but is also found in cardiac muscle and in adipose tissue, and helps GLUT-1 transporters get even more sugar and storage carbohydrate into these areas.
So think of it this way: insulin causes fat cells and muscle cells to soak up energy, and if your muscle cells are already “full”, which is often the case if you're not incorporating the strategies you’re about to discover in this article, then most of the sugar winds up getting driven into fat cells.
But here’s the amazing thing: just like insulin can upregulate sugar transporters, exercise can also upregulate GLUT-4 sugar transporters, but without an actual release of insulin from the pancreas. This means fewer chronic disease risks related to constant surges of insulin, less pancreatic strain, and a higher likelihood that carbohydrate and protein energy from food get partitioned into skeletal muscle and cardiac muscle rather than into adipose tissue. Exercise can even increase not just the activity, but also the number of GLUT-4 transporters you have available.
Of course, as you probably already know, physical activity can do much more than just play around with your sugar transporters, and can also mobilize fatty acids from your adipose tissue to be used as energy, increase your sensitivity to insulin when it does get released, and cause a host of other extremely helpful metabolic adaptations that make it one of the most powerful “drugs” on the face of the planet.
Now let’s look at five highly effective ways to maximize these blood-sugar controlling benefits of exercise as well as one non-exercise related way to control blood sugar.
Blood Sugar Control Strategy #1: Strength Train
Before diving into the concept of how strength training stabilizes blood glucose, it’s important to understand the concept of “glucose threshold”. The glucose threshold is the point at which sugar output into the bloodstream (e.g. from sugars in your diet, sugars that get broken down and released by your liver, etc,) and uptake (e.g. sugar getting driven into muscle) are in balance: if you are above the threshold, then glucose levels rise and you have high blood sugar, and if you are below the threshold, your blood sugar levels fall or stay the same. You can read more about glucose threshold and blood sugar levels in this study.
Research has found that when you strength train, your ability to drive glucose into muscle tissue from strength training occurs, and thus your ability to cause a decrease in your glucose threshold can occur when you lift weights that are at least 30% of your single repetition maximum weight (1RM). This is (surprisingly) not that heavy or difficult and means you can control blood sugar and upregulate sugar transporters with even relatively light bodyweight exercise.
Let’s take a closer look at this study. In it, test subjects (both diabetic and non-diabetic overweight middle-aged men with previous resistance exercise experience) were assigned to either a low or a moderate intensity protocol. Both protocols consisted of a weight training circuit of 3 sets of 30 repetitions of six basic weight training exercises that you're probably familiar with or can easily find at a gym: leg extension, bench press, leg press, lat pull down, leg curl, and seated row. Subjects recovered for 15-20 seconds between exercises, and then for a full two minutes between circuits. Weights were set at 23% of one repetition maximum (1RM) for the low-intensity group, and 43% of 1 RM for the moderate intensity group. Blood sugar and rating of perceived exertion (RPE) were measured both between sets and at 15-minute intervals during a two-hour post-exercise resting period. Subjects also ate a 285-calorie breakfast two hours before the test.
Blood sugar levels in the non-diabetic subjects fell initially during exercise, then rose after exercise as the body released some sugar into the bloodstream to support the exercise (a process known as glycogenolysis), then leveled off again.
No surprises there.
In subjects with type 2 diabetes, both the low and moderate intensity circuits lowered blood glucose, but surprisingly, the low-intensity circuit produced lower glucose levels, along with a lower rating of perceived exertion accompanied by less metabolic stress. This finding should be particularly relevant to overweight or untrained individuals who are just beginning a blood sugar management program, or for people who just feel too “tired” to exercise before or after a meal, because it means that even a single session of low-intensity resistance exercise at a relatively easy weight can offer significant benefits for blood sugar control.
Before leaving the topic of strength training for blood sugar control, it is important to understand that if you're already a relatively fit person the heavier and more intense your strength training, the more rapidly you will deplete muscle and liver glycogen levels, the higher your post-exercise metabolic rate will be, and the greater your amount of blood sugar control will be, so you eventually should progress to workouts such as a heavy 5×5 protocol or any of the other strength training strategies I describe here. But it’s also important to realize that even light weight training will suffice for basic blood sugar control.
Blood Sugar Control Strategy #2: Pre-Breakfast Fasted Cardio
A study published in The Journal of Physiology suggests a second, potent strategy for controlling blood sugar, especially in response to a meal: exercise before breakfast, particularly in a fasted state.
In this study, researchers in Belgium recruited 28 healthy, active young men and began stuffing them with what would be considered a pretty poor diet – a diet comprised of 50 percent processed, unhealthy fat (we’re not talking extra virgin olive oil and avocados, but more like soy and lard and the other nasties fed to subjects in laboratory studies) and 30 percent more calories than the men had been consuming prior to the study. A portion of the men (the control group) did not exercise during the experiment, and rest of the subjects were assigned to one of two exercise groups, working out four times a week in the mornings by running and cycling at a hard intensity for 60-90 minutes.
Now, here’s the kicker: two of the groups – the control group and just one of the exercising groups – were fed a huge, carbohydrate-rich breakfast. In the case of the fed exercising group, this meal occurred before exercising and then they continued to ingest carbohydrates (in the form a sports drink) during their workouts. But the second group exercised without eating and drank only water during the training. The researchers did, however, make up for the abstinence of calories in this second group by matching their energy intake of the first group with a big breakfast later that morning after training, a meal exactly comparable in calories to the fed group’s big pre-exercise and during-exercise portions.
The experiment lasted for a total of six weeks. At the end, the nonexercising group had, not surprisingly, packed on an average of more than six pounds of fat. Furthermore, they also developed insulin resistance, meaning their muscles were no longer responding to insulin and weren’t pulling sugar out of the bloodstream efficiently, resulting in the storage of extra fat in both adipose tissue and within intramuscular fat stores.
And the men who ate breakfast before exercising gained weight, too, although only about half as much as the control group. But somewhat surprisingly, just like the sedentary eating group, they also became more insulin-resistant and were storing away a greater amount of fat.
You’re probably anticipating what comes next. Only the group that exercised before breakfast gained nearly no weight and showed zero signs of insulin resistance. In addition, their metabolic rate changed in such a way that they also burned the fat they were taking in far more efficiently (a higher rate of fat oxidation). The study’s authors concluded “that exercise training in the fasted state is more effective than exercise in the carbohydrate-fed state to stimulate glucose tolerance despite a hypercaloric high-fat diet.”
And what was one significant characteristic of that pre-breakfast exercise group? You guessed it: increased levels of the muscle protein GLUT-4, which, as you may recall, is responsible for insulin-stimulated glucose transport in muscle and plays a pivotal role in the regulation of insulin sensitivity.
So…exercise before breakfast? Yep. Here's my morning routine and how I do it.
One last note here: should a 60-90 minute pre-breakfast exercise session seem daunting to you, you should be aware of another study review entitled “The impact of brief high-intensity exercise on blood glucose levels”. In this study, researchers investigated the effect on insulin sensitivity and blood glucose from a relatively small amount of high-intensity exercise – just 7.5 to 20 minutes per week. They found that two weeks of sprint interval training increased insulin sensitivity for up to three days after the exercise session! Furthermore, they found that twelve weeks of near maximal intensity interval running (for a total exercise time of 40 minutes per week) improved blood glucose to a similar extent as running at a lower, aerobic intensity for 150 minutes per week. In type 2 diabetics, they found that a single high-intensity exercise session improved postprandial blood glucose for 24 hours, while a 2-week high-intensity exercise program reduced average blood glucose by 13% at 48 to 72 hours after exercise and also increased GLUT4 transport protein expression by 369%! The researchers concluded that:
“…very brief high-intensity exercise (HIE) improves blood glucose (BG) 1 to 3 days postexercise in both diabetics and non-diabetics. HIE is unlikely to cause hypoglycemia during and immediately after exercise.”
So there you have it. When it comes to blood sugar control, there’s no need to hop on the treadmill for a full, epic hour and a half. You can simply do brief, high-intensity exercise, and here’s a full article I wrote that reviews some of the best, most up-to-date research on what kind of exercise counts as high intensity. Finally, not from peer-reviewed research but from my own testing with a blood sugar monitor, I've even found something as simple as a 30-minute easy walk in the sunshine, a yoga session or a relatively short, easy, aerobic effort can significantly lower post-prandial blood sugar levels after breakfast…
…and the effects are even more pronounced with the addition of morning green tea or caffeine, along with a cold shower or other form of cold immersion or cold gear use afterwards.
So now you've got zero excuses, eh?
Blood Sugar Control Strategy #3: Post-Prandial Walks
A few years ago, I was inspired to begin setting a rule to move or walk for at least a few minutes after each meal, even a late dinner, when I read an interesting Japanese study entitled “Postprandial lipemia: effects of sitting, standing and walking in healthy normolipidemic humans.”
This study compared the effects of sitting, standing and walking on postprandial fat storage in healthy Japanese men. The fifteen participants in the study completed three two-day postprandial trials (“post-prandial” means “after a meal”) in a random order: 1) sitting; 2) standing, and 3) walking. On day one of the sitting trial, participants rested. On day one of the standing trial, participants stood for six, 45-min periods. On day one of the walking trial, participants walked briskly for 30 minutes at approximately 60% of maximum heart rate. On day two of each trial, participants rested and consumed test meals for breakfast and lunch. The researchers then collected blood samples in the morning and afternoon on day one, and in the fasted state and at 2, 4 and 6 hours postprandially on day two. On day two, they found serum fat concentrations were 18% lower in the walking trial compared to the sitting and standing trials, proving that postprandial lipemia was not reduced when standing (or, of course, sitting) after a meal but was reduced after low-volume, easy walking for 30 minutes.
The study “Postprandial Walking is Better for Lowering the Glycemic Effect of Dinner than Pre-Dinner Exercise in Type 2 Diabetic Individuals” takes this science even one step further and looks at the effect of walking before a meal vs. walking after a meal.
In this study, twenty minutes of self-paced, easy walking done shortly after meal consumption resulted in lower blood glucose levels at the end of exercise compared to values at the same time point when subjects had walked pre-dinner. In addition, the investigators in this study found that one hour of aerobic exercise performed in a fasted state prior to dinner had a minimal impact on post-dinner glucose levels, but when performed two hours after the meal, induced a significant decrease in plasma glucose levels.
So, from what we know thus far, it looks like if you’re going to go on a walk at some point in the evening around dinner, you’re better off doing it after dinner rather than before dinner, and that you get benefits when it’s as short as 20 minutes (although I’d highly suspect you get benefits from any movement at all!).
The same study also makes another interesting observation about the timing of moderate aerobic exercise around a meal and the effect on blood sugar of this exercise: specifically, that postprandial, morning moderate intensity exercise decreases blood sugar levels after a morning meal, but this effect does not persist during and after the following lunch meal. This means that if you exercise in the morning, you’re probably going to still want to maintain at least low-level physical activity (e.g. a standing or walking workstation) between breakfast and lunch if you want to continue to reap the benefits of that exercise.
The study also reports that moderate bicycling exercise after any meal (breakfast, lunch, or dinner) results in a significant decrease in blood glucose levels and that both postprandial high-intensity exercise and longer bouts of walking (e.g. two hours versus one hour) reduce blood glucose levels and insulin secretion, suggesting that the effect of exercise is related more to total energy expenditure rather than to peak exercise intensity, leading the researchers to conclude that it is possible that the short duration of the exercise bout in this study (20 minutes) could have had a greater impact on blood sugar if either the intensity or its duration had been increased. This is backed up by the study entitled “Effect of Post-Prandial Exercise Duration on Glucose and Insulin Responses to Feeding”, which found that longer bouts of exercise after a meal produce a greater decrease in glucose and insulin.
Once again, sugar transporters play a big role here, and researchers reported that “the binding of insulin to its cellular receptors in muscle and adipose tissues recruits GLUT4 transport proteins to the cell surface that facilitates glucose transport. Muscular contractions themselves are known to stimulate glucose transport into muscle cells without the need for insulin through an independent mechanism, but in an additive manner, thereby potentiating the effects of post-meal exercise.”
So let's stop for a moment.
What do we know so far from all these studies? We know that one excellent strategy to control blood sugar would be to set a habit of exercising before breakfast in a fasted state, preferably using either longer aerobic exercise, brief high-intensity exercise or (if you're like me) even just a bit of yoga or a simple walk, and then, if time permits, to go on an easy 20-60 minute walk after dinner.
In addition, in tomorrow's podcast (episode #377 if you're reading this after the release) I'm giving you a full update on the latest research behind walking and fat loss, including the new finding that walking immediately after a meal is far more effective than waiting for an hour after the meal.
Blood Sugar Control Strategy #4: Standing
Using a standing desk can lower blood sugar levels, and there’s research to back it up!
In one study of office workers, standing for 180 minutes after lunch reduced the post-lunch blood sugar spike by 43% compared to sitting for the same amount of time. Interestingly, researchers noted that both groups took the same amount of steps after lunch, indicating that the smaller spike in blood sugar was due to standing rather than additional physical movements around the office.
Another office worker study discovered that alternating between standing and sitting every 30 minutes throughout the workday reduced blood sugar spikes by 11.1% on average. And yet another study showed that the harmful effects of sitting after meals, with excessive sedentary time post-meal at the office being linked to a whopping 112% greater risk of type 2 diabetes.
And that is why I not only recommend a standing or walking workstation, but also the incorporation of a concept called “greasing the groove”. This is a concept I originally discovered in a book called The Naked Warrior. The idea is basically this: Instead of (or in addition to) doing a long or hard workout at the gym, you simply spread your exercises throughout the day.
This not only allows you to become proficient at certain movements such as pull-ups or squas, but also elevates your metabolism throughout the day and gets you fit or maintains fitness without you needing to always set aside time for structured workouts. For example, I have a pull-up bar installed above the door of my office. Every time I walk under that bar, I have a rule that I have to do five pull-ups.
Other examples of “Greasing the Groove” that I include in my own life to become fit and control blood sugar even when I’m not exercising are:
-Beginning every day with a few minutes of yoga and calisthenics with deep nasal breathing…
-Doing 25 body weight squats or 100 squats every time I take a bathroom break…(caution: click here to see a hilarious video in which this practice got me into some serious trouble at an airport)
-Doing 30 burpees at least once per day…
-Doing 100 jumping jacks for every hour that I actually am sitting…
-Taking a cold shower 2-3 times each day…
You get the idea. Even during a day at the office, you don’t actually have to “workout” to be working out or to be controlling blood sugar. The trick is not be in one given position (including standing) for your workday, but to instead be in as wide a variety of positions as you can muster, including standing, lunging, kneeling, occasionally sitting with very good posture, balance boards, balance mats and other tactics I discuss here.
Whew! This has been quite a post thus far. You’ve learned why you need to control blood sugar, how sugar can wind up in either fat or muscle, why you should strength train (even at low intensities), the benefits of pre-breakfast fasted cardio, the benefits of post-evening meal walking, and the concept of staying active at the office with activities like standing and greasing the groove.
But I'm not done yet. At the times when you can't exercise, or when you need an added strategy to all of the above, there are quite a few natural compounds you can add to your diet to help control blood sugar and insulin spikes.
Blood Sugar Control Strategy #5: Plants, Herbs & Spices
Let's begin with cinnamon. Cinnamon has a long history both as a spice and as a medicine, and it’s unique healing abilities come from the essential oils found in its bark, which contain three active components called cinnamaldehyde, cinnamyl acetate, and cinnamyl alcohol. The cinnamaldehyde in cinnamon helps prevent unwanted clumping of blood platelets, which makes cinnamon anti-inflammatory.
In one study, the antioxidant effects of a cinnamon extract in people with prediabetes decreased a marker of oxidative stress by fourteen percent. Participants took 250 mg of cinnamon extract, twice per day, for twelve weeks. This is significant considering that chronic inflammation and oxidative stress plays a role in nearly every chronic disease, including diabetes.
Cinnamon also mimics the effects of insulin, which increases insulin sensitivity, making insulin more efficient at shuttling glucose into cells. Five grams of cinnamon is all you need to do this while also reducing total plasma glucose response. Effects last twelve hours. Cinnamon also reduces fasting blood glucose, total cholesterol, and triglycerides, and it increases HDL cholesterol. And the best type of cinnamon to use? Approximately the equivalent of 2 teaspoons of organic ceylon cinnamon per day will suffice. I like to buy it in bulk.
Gymnema Sylvestre is another potent herbal tactic for controlling glycemic variability. It has been used in traditional Ayurvedic medicine for thousands of years and has promising research around its ability to control blood sugar levels. Its blood sugar lowering effects are possibly due to it causing an increase in insulin secretion, which partially explains its ability to increase glucose utilization, with this also being due to it increasing the activities of enzymes responsible for utilization of glucose by insulin-dependant pathways. The increase in insulin secretion may be explained by Gymnema supplementation regenerating pancreatic islet beta cells, the cells responsible for sensing sugar in the blood and telling the pancreas to release the proper amount of insulin to maintain normal blood sugar levels. Gymnema also inhibits glucose absorption from the intestines and has been shown to lower serum cholesterol and triglycerides.
Gymnema Sylvestre extract administered to non-insulin-dependant type 2 diabetics at 400 mg per day for 18 months significantly reduced blood sugar, hemoglobin A1c and glycosolated plasma protein levels, with many participants lowering their diabetes medication and five participants ending with controlling blood sugar using Gymnema Sylvestre extract alone. The same reductions have occurred in people with type 1 diabetes, with Gymnema also allowing for a decrease in insulin requirements. The easiest way to use Gymnema Sylvestre is by taking one 400-600 mg capsule, standardized to contain 25 percent gymnemic acid, ten minutes before a carbohydrate containing meal.
Berberine, a compound derived from a variety of herbs including goldenseal and Oregon grape root, shows a variety of distinct benefits. It increases glucose uptake by the cells and improves insulin utilization by increasing glucose uptake pathways GLUT-4 and GLUT-1. Berberine also activates AMP-activated protein kinase (AMPK), with increased activation allowing for a reduction in fat storage, increased insulin sensitivity, reduction in cholesterol/triglyceride production, and suppression of chronic inflammation.
Berberine has also been shown to significantly reduce free fatty acids, high levels of which damage the pancreas and insulin production In one study, berberine significantly lowered fasting blood glucose, hemoglobin A(1c), triglyceride, and insulin levels in type 2 diabetics by increasing insulin receptor expression. It also improved liver function. Another study found that 500 mg of berberine taken twice per day by patients with type 2 diabetes lowered blood glucose, fasting insulin, and blood lipid levels.
There's a ton more research you can read here on berberine on everything from metabolic syndrome, PCOS, osteoporosis and much more. The standard dose of berberine HCL is 900-2,000mg a day, divided into three to four doses, taken with a meal.
Finally, I'm going to tell you about a compound I personally use daily to control my own blood sugar: bitter melon, also known as “goya” in Japan.
Bitter melon has only positives, as far as I am concerned. It’s fresh on my mind, because like I mentioned, when I was in New York City, I had the pleasure of spending quite a bit of time with Chef David Bouley, a world-famous Japanese cuisine expert who frequently travels to Asia to study specific food consumption and dietary habits that allow locales such as Okinawa, Japan to be such longevity hotspots. And one of the large bags of tea he brought back with him and gave to me was comprised of the same compound they ate in copious quantities before nearly every meal – you guessed it – bitter melon extract.
But I already knew of bitter melon because I’ve personally been using it in the form of a potent tiny capsule I'll fill you in on shortly, and I've been using it to manage my postprandial blood glucose levels with potent efficacy for the three years.
Taxonomically known as Momordica charantia, bitter melon may be effective in controlling blood sugar levels and regulating blood pressure. Although the precise mechanism by which it works (whether it’s through regulation of insulin release or altered glucose metabolism and its insulin-like effect) is not known, bitter melon naturally contains antidiabetic compounds like charantin, vicine, and polypeptide-p, plus some other health-boosting components like antioxidants.
Bitter melon is a popular treatment for diabetes and similar conditions among the indigenous people of Asia, South America, India, and East Africa. As noted earlier, it’s known particularly well in Okinawa, Japan. Okinawa, like the Bama County, is one of the world’s “blue zones”, an area where the average lifespan is unusually long, and it’s also where some of the longest-lived people on the planet live.
In places like Okinawa, almost every part of the bitter melon has been used in traditional medicine, including the fruit, leaves, vines, seeds, and roots. It’s used to treat everything from microbial infections to digestive issues, stimulate menstruation, heal wounds, reduce inflammation and fevers, deal with hypertension, and it’s even been used as a laxative and emetic. It also activates cellular machinery to regulate energy production (particularly AMP-activated protein kinase) and the way fats are processed by the liver.
Centuries of oral consumption have demonstrated that bitter melon is both safe and effective. And on top of all those other conditions, according to a number of animal studies, it can even reduce insulin resistance and protect against diet-induced hyperglycemia and hyperinsulinemia. It should be noted, though, that commercially-sold varietals are not nearly as effective as wild bitter melon. One study observed the effects of bitter melon on diabetic rats. Specifically, they used an aqueous extract powder of fresh, unripe melons, and found that a dose of 20 mg per kilogram of body weight reduced fasting blood glucose levels by 48%.
Part of the reason bitter melon is so darn effective is likely its effect on GLP-1 secretion. GLP-1 is glucagon-like peptide-1, a peptide released from what are called L-cells, which increase in density along the length of the intestines. It helps to raise insulin levels as a part of the incretin effect, a hormonal response that effects insulin secretion following oral glucose ingestion. A study was done to examine the role of bitter melon extract in this process, and found that through bitter taste receptors and/or a PLC β 2-signaling pathway, the melon stimulated GLP-1 release, which contributes, at least in part, to the antidiabetic activity of bitter melon through the incretin effect.
Now, before you think that by supplementing your diet with bitter melon, your insulin levels will get too high, it’s important to note that insulin levels that are regulated by GLP-1 are either reduced or, in some cases, completely absent in people suffering from diabetes. Considering that, and the fact that GLP-1 has an extremely short half-life due to rapid inactivation, it’s not likely that your insulin levels will become abnormally high by using the melon. In all likeliness, your insulin count will rise and settle at a relatively normal level. However, further studies will need to be performed to confirm this.
And there’s more.
Bitter melon, specifically a wild species called Momordica charantia Linn var. abbreviata ser., can also regulate inflammation due to various diseases. Wild bitter melon and bitter melon extracts were used in a study to inhibit macrophage activity, which is a part of your natural immunological response to stress, disease, and tears in body tissues. The lipopolysaccharide (LPS)-stimulated macrophages that were targeted responded to both extracts, but especially to the wild variety of the melon, resulting in much-reduced inflammation.
As you may already know, insulin resistance is closely related to chronic inflammation induced by things like tumor necrosis factor-α (TNF- α), a compound that seeks out and destroys cancerous cells. But before jumping into the importance of TNF- α, you should memorize this chemical: triterpene 5β, 19-epoxy-25-methoxy-cucurbita-6.23-diene-3β, 19-diol – or, for short, EMCD. It’s purified from a wild species of bitter melon that was thought to activate AMP-activated protein kinase (AMPK), which itself is thought to repress TNF- α-induced inflammation.
When it was tested alongside a compound extracted from green tea that’s also reported to be anti-inflammatory, EMCD showed more obvious anti-inflammatory activity, but not by activating AMPK. It actually inhibited the activation of the IkB kinase, an important aspect of pro-inflammatory signaling, and thus, the melon extract mitigated inflammation tied to diabetes. Since inflammation is connected to shorter life spans and greater risk of conditions like cardiovascular diseases, you should definitely look into adding wild bitter melon to your diet or supplement cabinet as an anti-inflammatory strategy too.
Want more interesting reading on bitter melon extract? Check out these links:
Going WILD with Bitter Melon for Blood Sugar Support
Is the Metabolic Syndrome a Consequence of Aging?
So how does wild bitter melon promote fat burning, liver health (and of course, anti-aging)? The answer involves caloric restriction and insulin.
Wild bitter melon has been found to activate cellular machinery to regulate energy production (technically AMPK-activated protein kinase) and the way that fats are handled by the liver. Activation of this metabolic pathway is important to aging. It is sometimes referred to as “exercise in a bottle” because activation of AMPK is an aspect of the benefits derived from exercise. The effect of an extract from the wild genotype of bitter melon has proved to be more powerful than others on the market and much more consistent in producing positive results.
Summary
So how can you get your hands on bitter melon extract?
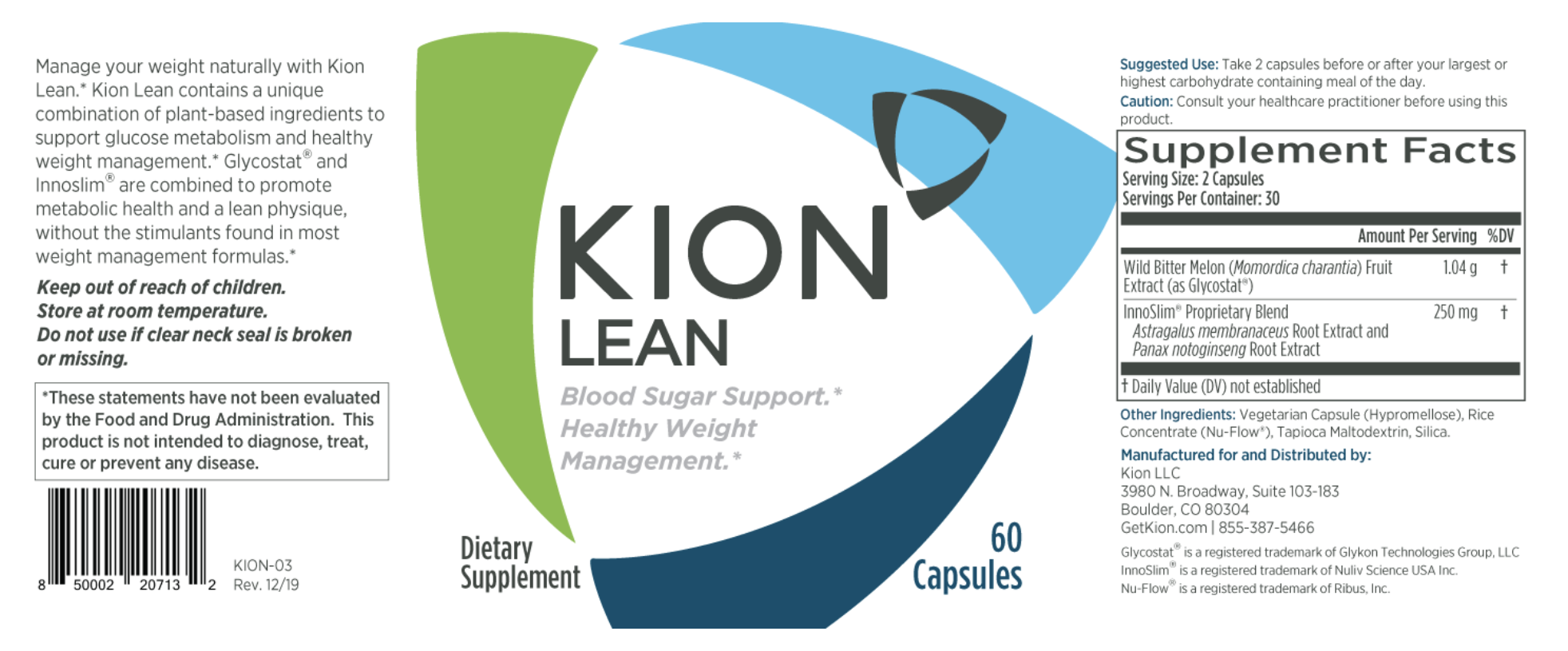
Simple: it's one of the main ingredients in the brand new formula now available as Kion Lean.
Kion Lean is a proprietary formula designed to assist with weight management and healthy longevity by combining the benefits of wild bitter melon extract and InnoSlim® (a blend of highly purified and fractionated Panax notoginseng and Astragalus membranaceus.) These potent nutraceuticals have been shown to decrease glucose absorption and circulating blood glucose.
That means fewer blood sugar spikes for you. InnoSlim® may also reduce fat accumulation by helping correct the metabolic issues that lead to weight gain.
to support:
- Healthy liver function, which comes in handy if you like your wine, beer or cocktails with your meal.
- Blood sugar regulation even if you can't exercise before a meal or hunt down cinnamon and vinegar.
- Healthy body fat levels without the use of harsh central nervous system stimulants like high-dose caffeine or ephedra.
- Anti-aging factors associated with longevity, without negative side effects.
You can click here to try Kion Lean now, and I’d recommend using it exactly as I do – two capsules before any carbohydrate-rich meal. It’s that simple.



Do you still do all of these things – or is there more research and updated information? I have just been told I am pre-diabetic…I am searching the net to save my health.
500mg Berberine before bed will it help with fasting glucose levels ? speed up results of fat loss / cell turn over ?
Hey Ben! Stumbled upon this article while doing some research for my own book. As with other presentation and Q&A’s that you’ve done, was “A Biohacking Adventure: 7 Culinary Tactics For Enhancing Health & Longevity” you did in NYC recorded and available anywhere? Or was this a private presentation? Thanks.
In regards to the herbs and spices recommended, would you take all the recommend doses prior to each meal? How would you suggest taking each supplement? Kion lean, cinnamon, berberine, etc all at once? In fasted state, only before eating carbs? Chance of going hypoglycemic? Thanks for your time and can not wait for the new book!
I believe all of the recommendations are in the article. If you still have questions, I'd be happy to help via a one-on-one consult. https://bengreenfieldfitness.com/coaching
Great read Ben. I’m working in N. Iraq these days & trying to keep up w/the heat while working out is always a challenge. Every year before I head back home to U.S. for a month I always amass a new list of potions/powders/tinctures, etc. to bring back w/me to keep me going for another year so I’ve some new ideas from you now- especially cinnamon & bitter melon.
Thanks for the article, nice read. How do you recommend using apple cider vinegar (before/post meal, quantity..) taking into account its acidity you`ve mentioned earlier?
I drink 1tsp of ACV in water with a straw (to protect tooth enamel) in the morning and before meals.
ACV can stimulate stomach acid, which is why it’s a good pre-meal digestif. 1 teaspoon to 1 shot ACV prior to a meal to reduce blood glucose response to meal is perfect. Can be mixed with sparkling water and stevia.
As far as whether or not it’s acidity matters *internally* depends on who you ask, but I think most health professionals now know that the pH of food doesn’t directly affect your internal pH (e.g. acid vs alkaline). Good article here: https://www.healthline.com/nutrition/vinegar-acid…
I really hate doing anything after having a meal – especially a good one – other than sitting or lying down :)
Anyway, there’s a lot of interesting information and tips in this article so thanks for taking the time to put it all together!
No kidding aside- does sex count as post dinner excercise?
I was thinking that haha
Great article.
Re ‘#2: Pre-Breakfast Fasted Cardio’, does a sauna session count? 4 days a week, pre-breakfast, I do a 20-minute session in a dry sauna (avg temp 180F).
Yep, that counts, although I tend to do yoga during my sauna to elevate HR.
Thanks for the reply. The sauna just keeps giving and giving. It’s definitely among my top 5 biohacks.
Hey Ben!
Great article!
Would you mind sharing what it was that indicated that you are at greater risk for Type II Diabetes from your genetic test?
Studies have identified at least 150 DNA variations that are associated with the risk of developing type 2 diabetes: https://ghr.nlm.nih.gov/condition/type-2-diabetes… – and here are a few such snips: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3746…
Nice article, thanks…As long as it’s not hydrogenated, what’s wrong with lard?
Well, check out the horrible quality of these mice-fed diets: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2394…
What’s your height and weight in your men’s health feature?
6'2 180!
An excellent read. Thanks, Ben.