May 19, 2020
You may have heard me talk about, in last week's podcast with Biological Dentist Dr. Dominik Nischwitz, how I would never step foot near a “regular” dentist's office.
This is because I understand how profound an impact my teeth, gums, tongue, and oral cavity have on my entire biological system—so, I only work with a holistic, biological dentist.
And after speaking with Dr. Nischwitz, I am even more convinced that every person seeking to optimize his or her health absolutely must first optimize their oral health—and working with a biological dentist is the first step in doing so.
Dr. Nischwitz is a world specialist in biological dentistry and ceramic implants, the president of the International Society of Metal Free Implantology, and co-founder of DNA Health and Aesthetics, Center for Biological Dentistry. He recently published the book It's All in Your Mouth: Biological Dentistry and the Surprising Impact of Oral Health on Whole Body Wellness (which I highly recommend checking out) and he also penned today's article.
In short, you're about to discover why hidden oral issues are causing an epidemic of chronic health problems and what to do about it, and it also takes a deep dive into the problems with conventional dentistry, how oral issues can cause chronic inflammation, how “interferences” are affecting your overall health, the problem with root canals, why it's imperative to work with a dentist who knows how to safely remove such interferences (and what to replace them with), the oral microbiome, and much, much more.
The Problem With Conventional Dentistry
The primary focus of most traditional dentist offices (the ones Ben won't set foot in) is on the repair and maintenance of teeth, and even more specifically centers on biting.
In a way, this classic approach makes total sense as teeth, when fully developed, do not change all that much. So keeping them in the same state is a logical means to maintaining the ability to chew fully and consistently throughout your life.
But because dentists throughout history haven't been trained as medical doctors (rather as craftsmen), this view of only maintaining a proper bite, repairing teeth, and treating pain locally is still the way they get trained in dental school today and can lead to a myriad of problems that you'll discover in this article.
It is not uncommon to see a cyst (a sign of chronic inflammation) on the tip/apex of a root canal treated tooth (often the size of a pea!) and the only question that is asked by a traditional dentist is “Does it hurt?!, No?, OK, we’ll just keep on monitoring it!” instead of trying to figure out the root cause and removing it (the cause and the issue).
Thus, the important connection between a chronic, silent inflammation in a patient's mouth causing a pro-inflammatory state throughout their whole body, unfortunately, is rarely made. This is why it is critical to remember (as all biological dentists are taught) “The mouth is a mirror of overall health.” If you have issues there, you’ll have them somewhere else in the body too as a result.
How “Interferences” Can Cause Chronic Inflammation
Health issues that tend to fly under the radar can become 24/7 chronic stressors that put a significant strain on your hormones, immune system, health, and performance—without you even knowing it. Oftentimes these stressors start in the mouth, and by removing them, you can boost your health extremely quickly because after all, health starts in the mouth.
Biological dentistry could very well be the missing piece of the puzzle that you've been searching for to flourish and live a healthy, happy life.
Your mouth is the gateway to the rest of the body, and whatever gets put in it gets transported (or has an impact on) the rest of your body. This can include food, cosmetics, metals, toxins, and more.
The field of biological dentistry is even more aware of this than all other areas of the health and medical world because a biological dentist knows that dentistry isn’t just about repairing one tooth after another, it’s much bigger than that. Biological dentistry is all about making the body as healthy as possible by freeing it from anything that is likely to disturb, poison, or make it ill; or in other words, rid the body of anything that can cause inflammation.
We call this removing “interferences” and believe that if health starts in the mouth, then health optimization does too. This realization can be the salvation for chronically ill people; and for others, it can be a strong step toward much better efficiency with health and higher performance.
As soon as chronic inflammation, metals, or other interferences are removed from the body, the overactive immune system is relieved and the body often feels as though it’s finally able to “breathe” again. Often, it then switches from sympathetic mode (fight or flight) to parasympathetic mode (rest, digest, and repair). The parasympathetic mode is the only program in which the immune system is able to function properly, and where regeneration and restoration can take place.
The immune system is designed to repel bacteria, fungi, viruses, and other microorganisms. In Western countries and industrialized nations, there is currently an epidemic of chronic systemic diseases. There are many causes, but hyper-reactivity of the innate immune system with proinflammatory cytokines like TNFalpha, IL-1beta, IL-6 and NFkappab being produced chronically, plays a crucial role in this equation.
After these interferences are removed, many of my patients experience this state of rest, digest, and repair for the first time in years and report back that they can feel a significant change.
Your teeth are more like your liver, stomach, or intestines than you might think—they are organs with their own blood and nerve supply and are attached to a very important cranial nerve, the trigeminal nerve.
Teeth are directly connected to the vagal nerve and therefore connected with the autonomic nervous system. They are also the organs that are anatomically closest to the brain, which is a super important thing to note.
This is why highly toxic materials (which are classified as interferences in biological dentistry and functional medicine)—that are routinely embedded in this super-sensitive area under the guise of a durable filling—like mercury can often present serious consequences for your entire body.
According to world-renowned integrative medical specialists like Dr. Dietrich Klinghardt, Dr. Thomas Rau, or Dr. Thomas Levy, about 70% of all interference fields in the body are in the oral cavity. Apart from classic problems such as cavities and periodontitis, there are 5 primary interferences I'll discuss in this article:
- Metals
- Root Canal Treatments
- Cavitations
- Biting problems
- Imbalanced Oral Microbiome
Let's take a deeper look at some of these interferences.
1. Metals
Metals used in dentistry are inherited burdens from the previous century. For different metals such as mercury, gold, platinum, copper, cobalt, aluminum, iron, and chrome, the cytotoxic (neurological diseases), immunological (autoimmune disorders), and mutagenic (cancer) effects, as well as effects on the heart are scientifically well documented.
Metal components can usually be detected throughout the entire body just a few days after installation in the mouth.
Besides an obvious look into the mouth (for visible metals), the gold standard in testing heavy metals is the urinary heavy metal challenge, which is usually performed under the supervision of a medical or naturopathic doctor by using a chelator like ethylenediaminetetraacetic acid (EDTA), dimercaptosuccinic acid (DMSA), or 2,3-Dimercapto-1-propane sulfonic acid (DMPS). It should not be done at the beginning and never when there is any metal still installed in the mouth because this can wreak total havoc on the body and actually make matters worse. First, you must remove the source! Other heavy metal tests like blood and hair analysis are available like Dr. Chris Shade's Tri Test for heavy metals for a not so invasive initial measurement.
Amalgam (otherwise known as highly toxic hazardous waste) is an alloy of mercury with various other heavy metals like silver, copper, or tin that is solid or liquid at room temperature according to the proportion of mercury present, and is used in making tooth cements. Even today, amalgam is routinely used in most dental practices. On the one hand, this is because it is a material that is easily processed and lasts for a long time, and on the other, because it is subsidized by health insurance companies and is therefore free.
Mercury is considered the most toxic non-radioactive element, and thus exceeds all other known elements such as lead, cadmium, and arsenic, in some cases many times over. It has been completely banned in Norway and Sweden, which of course also includes fillings composed of the metal. In Russia, amalgam was already abolished completely by the end of the 1970s.
In dental practices, amalgam must be disposed of after removal as highly toxic hazardous waste—this fact alone should give pause for thought. Amalgam consists of 50% mercury, which contrary to what is often assumed, is not firmly set in the filling after mixing. Can you see a reason to risk having this in your mouth?
Basically, there are three different metal-related challenges or problems for the body to be aware of:
1. The toxicity of the metal: The highly toxic amalgam (contains 50% mercury) particularly plays a prominent role here. All heavy metals like mercury, lead, tin, aluminum, and cadmium are able to bind to sulfur-containing proteins, enzymes, cofactors, and cell membranes. This covalent bonding can completely block the function of important enzymes. Enzymes are needed for pretty much every function in your body—nutrient absorption, protein synthesis, bone-building, detoxification—and are an integral part of receptors (which are mostly proteins too) such as insulin or vitamin-D receptors, or a nutrient transport protein like GLUT-5, which could lead to insulin resistance, fructose-intolerance, or a whole host of other detoxification impairments. Over time, your body will become depleted in various crucial nutrients like methyl-donors and glutathione.
Moreover, metal ions from all dental alloys dissolve in an aqueous medium like saliva and thus corrode, increasing the toxic burden on your body. It also results in a flow of current which is called the galvanic element, or more simply put: a battery. Electrogalvanism, and the resulting electrical sensitivity, can frequently be the cause of a lack of concentration, memory loss, sleeplessness, non-specific symptoms such as a sharp pain or pressure in the chest, unexplained tachycardia, tinnitus, and hearing loss…just to name a few.
Chewing, grinding, brushing your teeth, or simply consuming hot or cold beverages release a certain amount of mercury vapor every day. All of this takes place within the microgram range; however, if one considers that even one molecule of mercury can destroy nerve cells, this cannot be underestimated. A study by Leong and Lorscheider showed that inorganic mercury quantities of 0.02 ng Hg/g led to the complete destruction of the intracellular microtubules and to a degeneration of nerve axons. In animal studies, after 14 days of amalgam wearing time, pathological changes could already be detected in the brain.
The human body is extremely intelligent and stores, wherever possible, fat-soluble toxins in the metabolically inactive connective or adipose tissues. However, in athletic people or those with a low percentage of body fat, the toxins are frequently deposited in the nerve tissue or brain.
In the gastrointestinal tract, the mercury from amalgam is converted from microorganisms into the organic, methylated form. A 2 to 3-fold increase in organic methylmercury was exhibited in the saliva of amalgam carriers compared to subjects without amalgam. Fish consumption was identical in the two groups in both quantity consumed and frequency. Methylated mercury in the gastrointestinal tract seems to be much more toxic than methylmercury from fish consumption since the mercury in the fish is already bound to amino acids, whereas it is directly formed in the body and is thus is clearly more reactive.
Since amalgam fillings are the main source of mercury (and other heavy metal) poisoning, they should be removed either in the event of chronic illness or for preventive reasons.
2. The immunological component: None of the dental metals actually have a positive biological function in the human body. They’re not supposed to be there, and as a result, every metal is seen as a foreign body by the immune system, and thus, can trigger an allergic reaction. This process is individual and completely independent of the quantity or number of metal crowns, inlays, or metal implants. The cell forms antibodies to the metal or the compound resulting from the metal and cell (Hapten effect), which plays an important role in the development of autoimmune diseases such as MS, Hashimoto Thyroiditis, etc. Essentially, your body is constantly fighting the foreign object.
3. The electrical component: In today's age of mobile phone transmission, WIFI, radar, and various wireless networks used by the military and others all beaming around us 24/7, we are all inevitably bombarded with different frequencies and forms of electromagnetic radiation (3G, 4G, 5G). Any metal restorations and titanium implants used in the oral cavity act as small antennas with transmitter and receiver effects which can interfere with your nervous system. The radiation is amplified in an uncontrolled manner resulting in the heating up of surrounding tissue. The standard absorption rate of electromagnetic fields can be increased 400 to 700-fold through the use of a cell phone (ringing or SMS reception) in combination with metals in the mouth. This study shows the release of mercury from dental amalgam restorations after magnetic resonance imaging following mobile phone use. We’re electrical creatures, and this intensified EMF messes with electrical signals that make our bodies work as they should. The effects on the body are therefore uncontrollable, and unmeasurable.
If you'd like to take a deeper dive into the dangers of heavy metals in your body (and learn solutions for detoxing), here are some of Ben's podcasts and articles to check out:
- How Hidden Sources Of Heavy Metals Are Destroying Your Health, And What You Can Do About It.
- The Crucial Do’s And Don’ts Of Heavy Metal Testing And Metal Detoxification.
- How Hidden Sources Of Heavy Metals Are Destroying Your Health, And What You Can Do About It.
- Special Episode: How I’m Going To Completely Detox My Body In 2018 (Detox Myths Busted, Detox 101, Advanced Detox Strategies & Much More!)
- How to Protect Your Body from the Ten Hidden Killers in Your Home (Fully Updated Version).
- The Most Effective Detox You’ve Never Heard Of (And Exactly How To Do It).
2. Root Canals
Two things biological dentists do not like to see are dead teeth and teeth that have undergone a root canal treatment (as they are dead too!).
This is not just a whim of biological dentists; in the medical world, it is universally accepted that no other medical discipline tolerates dead body parts being left in the body. This should include teeth, but it doesn't. This seems crazy to me.
In the medical world, dead body parts are removed as quickly as possible because of the inflammation they can cause and the toxic risks they pose to one's health. A root canal treatment can initially provide relief, and certainly contributes to the disinfection process in the short term, but sooner or later, a dead or root-canal-treated tooth (see photo below) will be repopulated with bacteria; and, as a result, will always lead to chronic problems in the body. Root canal treatments do have their place though, and should only ever be used for short-term, acute pain treatment.

As you can see, this is not a healthy body part. Root-canal-treated teeth are chronic inflammatory sites that can lead to chronic problems locally, but more often in other areas of the body as well. More than 100 years ago Weston Price already coined the term “focal infection” for this purpose. Without a blood, nerve, and lymph supply the tooth is only dead organic tissue with no immune function—which, thanks to its anatomy represents the perfect cavity for pathogenic microorganisms. There are between 30-75,000 “dentin canals” per square millimeter. If all the dentin canals of a root were lined up, they would cover a distance of approx. one kilometer. Pathogenic bacteria exist in this widely ramified canal system of a root and form highly toxic sulfur compounds (thioethers, mercaptan), which can block vital enzymes at their active center. As nonliving organic tissue can begin to decompose over time, necrogenic material with increased toxicity (putrescine and cadaverine) can also develop. As a result, it’s important to remove all possibilities of infection because the immune system won’t be able to reach, nor recognize it.
The nonspecific innate immune system reacts to this infectious site with the increased production of pro-inflammatory cytokines (TNF-alpha, IL-1beta, IL-6, Nfkappab). This leads to chronic inflammation systemically, as well as of the surrounding tissue locally.
It is also common for a patient to have an allergic reaction to root filling materials which usually contain classic allergens such as epoxy resin, Peru balsam, or rosin.
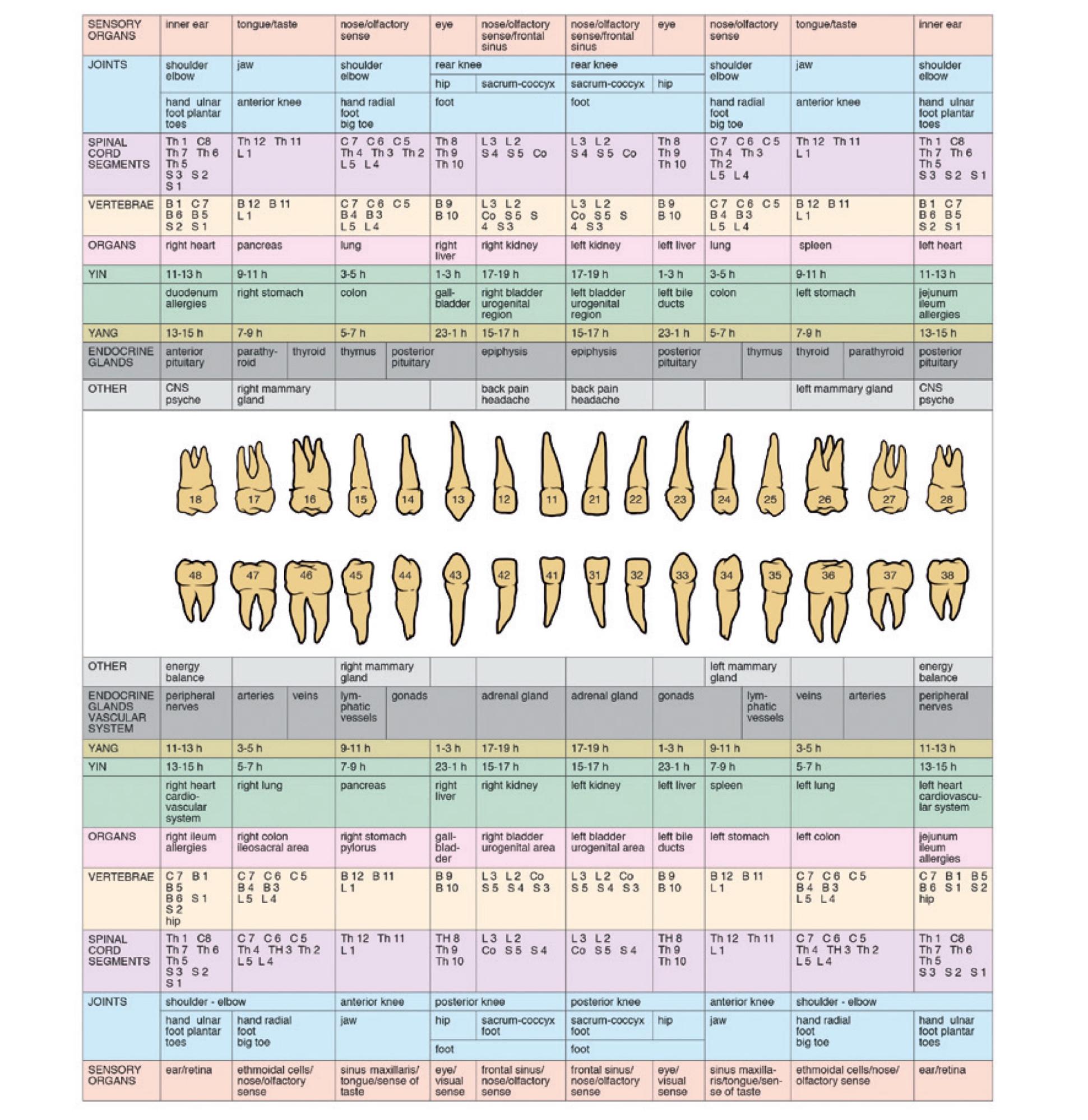
Teeth and their periodontium have a relationship with other physical structures and organs. Reinhold Voll coined the term “odonton,” the tooth meridian connections you'll see in the graphic below and identified (with electro-acupuncture) the direct and close interrelations between individual teeth and the different areas/organs of the body.
Interactions of positive and negative influences are possible in both directions. I’ll explain.
A disturbed organ can pathologically affect the associated odonton, and conversely, a sick tooth (or its periodontium) can disturb its correlating organ. If you’ve had root canal treatment, this isn’t to say you need to panic. There’s no rush to remove every root-treated tooth immediately. That said, I recommend that anyone who has undergone treatment be critically questioned and examined for signs of inflammation or cysts at the root tips. A healthy body can usually tolerate chronic inflammation for a while until another solution is found.
When looking for a solution to this issue, it is always important to take into account the patient’s overall health and what their goals are. Do they need to be at the top of their game and stay completely healthy? According to a study from my colleagues Dr. Lechner and Dr. von Baehr, the data demonstrate that local pathologies caused by endodontically treated teeth may increase immunological and systemic dysfunction, which should at least raise an eyebrow in all folks who are interested in biohacking or optimizing their health!
For chronically ill people and high-performance athletes, I recommend finding an experienced biological dentist who can remove the diseased tooth (I'll list some resources for doing so in the summary below), thoroughly clean and disinfect the surrounding structures (with ozone and neural therapy), and as a bonus, replace the tooth with a ceramic implant immediately to ensure the gum and underlying bone doesn’t recede. I call this “socket-preservation 3.0.”
3. Cavitations
Cavitations, also known as fatty degenerative osteonecrotic jawbone (FDOJ), chronic ischemic jawbone disease (CIBD), or neuralgia inducing cavitational osteonecrosis (NICO) are chronic inflammations in the jawbone. Undetected by conventional x-ray, they often occur as a result of old, not optimally healed tooth extraction wounds, dental germs, or foreign bodies.
Wherever wisdom teeth have been removed (especially if the extraction took place during puberty), it is likely that these chronically inflamed extraction wounds have developed.
Similarly to endodontically treated teeth, toxic substances and inflammatory cytokines (TNF-α, IL-1beta, IL-6, RANTES) develop in the jaw, which can cause various symptoms systemically—neurological (NICO), joint, or gastrointestinal problems are particularly frequent. These can be well diagnosed on suspicion when using 3D digital volume tomography (DVT) and read by a qualified biological dentist, but in most cases not by a traditional dentist.
Anyone who is curious about NICOs or FDOJ can ask their dentist for a panoramic image (an X-ray), followed by a DVT 3-D X-ray. However, it’s important to go to a dentist who is familiar with NICOs and able to recognize their pathological structures. Dentists who are not trained to spot them will not be able to find them on an X-ray. On the positive side, those who are able to identify FDOJs are also able to treat them.
FDOJs can be removed using a minimally invasive surgical technique. The wound is cleaned out and disinfected with ozone using and a technique known as Piezosurgery, a procedure carried out with the help of ultrasound. In my practice, the wound area is then filled with APRF membranes. This is a biological material made from the patient’s own blood, which makes it highly natural and biocompatible. The procedure, therefore, draws upon a mechanism that the body would usually use to heal itself.
When the human body is injured, it generates proteins to accelerate the wound healing process. These can then be used for the production of natural tissues. A small amount of blood is taken from the patient and centrifuged then used to make a suspension fluid with a high concentration of platelets. These platelets contain the information required for tissue regeneration like various growth factors and even stem cells (about 1.2%). When these are placed in the wounded area of the treated FDOJ, they serve as a matrix for bone regeneration and also stimulate tissue regeneration.
4. Bite Problems and Dysfunctions of the Mandibular Joint
The chewing process is essential to our survival. In the last 100 years, innate and developmental abnormalities of the upper and lower jaws have become everyday occurrences. This seems to have primarily epigenetic causes, and notably, nutrition plays a crucial role here.
Food (mainly sugar and white flour products) seems to be directly linked to the development of malpositions of the teeth and jaw. Nowadays, it has become relatively rare in industrialized nations for a child or adolescent not to have some type of orthodontic device.
Dental occlusion and eye level are directly connected to one another and should be quite parallel to each other. In every mammal, the eyes are fixed on the horizon (labyrinthine righting reflex). Even the slightest changes in occlusion can lead to an imbalance in this structure. The compensation occurs through simple control mechanisms in the muscular and ligamentous apparatus, but initially through a shift of the cranium along the sutures and meninges. This mainly manifests itself in tension of the deep neck musculature. However, over a longer period of time, it is transferred onto the shoulder and pelvic girdle. Thus, in the long-term, misalignments and malpositions of the whole posture can develop.
This deep neck muscle tension also leads to a reduced blood supply to the brain in certain areas, as well as decreased blood flow and lymphatic drainage from the brain. Even a millimeter loss at bite level leads to a clear loss in lymphatic drainage and concomitantly to an accumulation of toxins in the brain area. Apart from the usual symptoms of craniomandibular dysfunction and myoarthropathy, a myriad of other symptoms can arise as a result, including concentration and memory loss (reduced supply of the neurotransmitter acetylcholine due to deficient blood circulation), migraines, sleeplessness, neck pain, pain in the lower back area, and even depression.
The mouth could be compared to a large building site that is never finished. Every day the body must expend workers and building material in terms of nutrients and ATP in order to compensate for this building site. As such, consistent biological cleaning of the oral cavity plays an important role not only for chronically ill patients, but also (if not more so) for everyone in terms of prevention.
Check out Ben's podcast on teeth care tactics or Chapter 17 of his book Boundless on maximizing your symmetry and beauty for more on strengthening your jaw.
5. Imbalanced Oral Microbiome
Generally, we think good oral health requires a mouth that is “clean,” or low in bacteria. In reality, our mouths are only healthy when they are teeming with thriving microorganisms. Stability and balance among the different types of microorganisms are far more important than sterility.
Despite the fact that the mouth is quite clearly the entrance to our gastrointestinal tract, scientists have taken a back-to-front approach in studying the digestive system, so to speak.
Many of the fascinating findings about our coexistence with bacteria have many come from examinations of the intestine. Gradually, however, scientists are starting to direct their gazes upward to the mouth and its impact on the intestines.
Anatomically, the mouth and the gastrointestinal tract are hardly distinguishable. Our mouths are not isolated units that simply stop after the uvula. In fact, the border between the mouth and intestine only exists in anatomy books. In real life, they make up an inseparable unit.
Every strain of bacteria in our intestine has made its way there via our mouths, and we now know that the microbial populations of oral and intestinal flora remain strongly connected throughout our lives. This is due in no small part to the fact that our saliva contains up to 109 microorganisms per milliliter, which make their way into the intestine each time we swallow. That’s one to three grams of bacteria per day.
The close connection between the mouth and intestines has many advantages for humans. Visibility is one of them. While it’s quite difficult to look at our intestines without a technical device to find out what’s going on in there, it’s quite easy to look inside our mouth. We simply have to open it and have a look. Just read Ben's article “What Your Tongue Is Telling You: 6 Important Clues Your Tongue Can Give You About Your Health.” for more information on how oral health is directly related to overall health.
Sometimes, it’s not even necessary to look inside the mouth. It’s possible to tell when someone has a health problem with their mouth simply by smelling it—bad breath is almost always an indication of an imbalance in the microbial community. An imbalance in the oral flora might smell acrid, sour, sulfurous, or—in the case of severe inflammation—like a festering open wound.
An entrance hall will usually tell you what to expect to find in the rest of the building. Our mouths work in the same way. If there is an unfavorable bacterial climate here because the gums or tooth root are chronically inflamed, or because bad tooth fillings are constantly releasing toxic substances, then this problem does not stop somewhere beyond the tonsils. Inflamed oral mucosa (leaky gum) always continues further down into the intestine. If the ecology of the mouth becomes imbalanced, this usually affects the remaining gastrointestinal apparatus as well. And what you see in the mouth usually continues into the gut.
Recently researchers discovered that inflammatory bowel diseases such as Crohn’s or ulcerative colitis may originate in oral microbiome. Scientists have found increased numbers of bacteria types that are usually found in the mouth in the intestinal microbiome of people with chronic diseases. It would appear that a particular genus of these bacteria can cause intestinal inflammation in people with a predisposition to particular diseases when they are swallowed with saliva.
The Importance of Proper Preparation Before Surgery
The general practice in standard dentistry is to operate on people more or less as they come into the clinic off the street. The only preparation for surgery is premedication or information about the treatment.
Any procedure/dental work, therefore, comes as a shock to the body.
The majority of postoperative traumas such as swelling, pain, and inflammation are not just side effects of the operation; they are above all evidence that the body is not able to compensate for the procedure.
Most people living in the Western world are in immunological hibernation. By that I mean that only the basic metabolic functions work (so that we don't die). This is due to the fact that many of us are poorly nourished because of our eating habits, the quality of factory farmed foods is low (including nutrient and mineral density), and the way in which our food is prepared is no longer adequate. Check out “How Factory Farming In America Is Producing Nutrient-Void Food (And How You Can Navigate Your Way To Healthier Options).” for more on how not to fall victim to this. Also, in winter we don’t get enough natural sunlight to make sufficient vitamin D for our immune system to operate as it should.
As with any surgical procedure, it puts the body under tremendous stress and requires a great deal of healing. To make sure my patients are able to compensate for this stress, and to optimize the regeneration process to avoid failure or recurrence, they are instructed to prepare for the procedure according to a very specific, individualized protocol.
Anything that could prevent bone regeneration after a tooth extraction, or the healing of the interference field or implant, should be avoided. This means that patients should pay attention to nutrition and avoid high quantities of sugar, grains, highly refined omega-6 oils, dairy products, as well as ensure they are not deficient in any vitamins or nutrients.
Before the surgery phase, the patient’s diet should be as hypoallergenic and anti-inflammatory as possible, while remaining high in nutrients.
When our bodies are deficient in nutrients, particularly amino acids, vitamin D3, and vitamin A, minerals (zinc and magnesium), trace minerals (save 10% on Quinton hypertonic solution with code: GREENFIELD10), omega-3 fatty acids, and other micronutrients, it can become overwhelmed by the combination of the deficiency and the healing process. This is because the body is unable to build new tissue as it simply lacks the nutrients it needs to do so. As a result, we encourage every patient to ensure they get the right (micro)nutrients and nutrition.
This isn’t important only for people undergoing a surgical procedure—it should be practiced by everyone at all times. The best thing a person can do for their teeth and overall health is to eat well. Hippocrates said it a long time ago: “let food be thy medicine.”
Removing Metals From The Mouth Safely
Amalgam fillings have been used in the mouth for many years now, but due to the enormous immunological and toxicological strain they place on our bodies (and because of modern advancements), these metals are no longer needed and no longer have a place in the mouth.
While all metals should be removed as part of a thorough biological dentistry or functional medicine treatment, this procedure should only take place under very carefully protective measures.
Unfortunately, it is when patients seek to have their amalgam fillings removed by non-biological dentists that most mistakes happen. Many of these traditional dentists are still too careless when dealing with amalgam, aren’t aware of the problems related to it, and may not see the need to take any special protective measures when removing it. As a result, some dentists put not only their patients in danger, but also themselves. Because large quantities of highly toxic, inorganic mercury vapor are released during the drilling process of removing amalgam fillings, this procedure can only take place under maximum protective conditions.
Some of the protective measures biological dentists use in their clinics (for all metal removals) include:
- Rubber dam: This protective rubber cloth is inserted over the teeth and covers right up to the back of the mouth. This protects the mouth from chips and fragments.
- Cleanup suction tube: This provides extra protection from mercury vapors.
- Careful drilling: Amalgam must be removed with the dental handpiece (also known as a dental drill) set at a low speed to avoid toxic mercury vapor from escaping. Ideally, the filling should be drilled in such a way that the majority can be taken out in one go, which prevents vapor from being released in the first place.
- Fresh air supply via a nasal probe.
- Air purifier: A special air purifier such as the IQAir can remove up to 99 percent of mercury vapor in the air. This is good for both the patient and the doctor.
- A dentist should always wear an additional FFP3 protective mask, which filters 99 percent of invisible mercury vapor.
- The insertion of chlorella algae once the amalgam has been removed absorbs any leftover mercury. Other options are possible such as activated charcoal.
- Infusion with high-dose vitamin C and other micronutrients reduces the immune response.
- Grounding during surgery (all of our dental chairs are grounded) for free electrons, to reduce inflammation, help relax the immune system, and promote healing.

Pictured above: Full set up of a safe amalgam removal. IQ Air purifier (to suck up 99% of the toxic mercury vapor), rubber dam, nasal probe, and special clean-up suction in place. Dentist and assistant are wearing FFP3 protection masks. Not shown: IV nutrients.

Pictured Above: Green latex-free rubber dam, special suction device called “clean-up-suction.” Amalgam “silver fillings.”
Ceramic Implants: The Metal-Free Solution
Despite low success rates, root canal treatments have prevailed for so long because there have been no good alternatives available. The other option was pulling the tooth out and inserting a dental bridge into the gap, later to be filled with a titanium implant.
As long as there is a hint of a chance of saving a tooth, most dentists will take it and do everything they can to make sure the tooth survives.
This is because dentists are traditionally trained to preserve teeth—and who wouldn’t be happy to hear “We can save the tooth!” The fact that saving a tooth can sometimes be at the expense of the patient’s overall health, however, is often overlooked.
Biological dentistry sees things the other way around. We don’t talk of teeth being sacrificed. Dentistry, technology, and implantology have made enormous progress in recent years. Diseased teeth can cause serious chronic diseases, but removing them has historically come at a high cost—loss of bone and gums, unpleasant aesthetics, comfort, time, money, and self-confidence were all at stake.
Today things are different because new, highly biocompatible materials are available. In biological dentistry, ceramic implants are the material of choice when it comes to filling a gap. If you’re wondering, “But does ceramic stay put?”—don’t worry. The material is a world apart from Grandma’s tea set. Today, we use high-performance ceramic made from zirconium dioxide, which surpasses metals in terms of stability and, above all, biocompatibility.
Finally, ceramics are on the rise more than any other material in dentistry, yet only around 1 percent of implantologists use ceramic implants. I have been doing ceramic implants for almost 10 years now and have placed over 3,000 pieces up to this date. That’s more than anyone else on the planet, except my mentor.
Ceramic implants do not conduct heat, which means the surgeon has to focus more on the condition of the bones. Additionally, they can only heal in a healthy body with healthy bones, which means the dentist carrying out the treatment needs to be very familiar with the correct healing process. Aside from these two constraints, there are many advantages to ceramic implants. Unlike gray titanium, they are free from metal and completely white.
But the most crucial factor for biological dentists is that they are completely neutral (as long as they aren’t dyed). This means they do not release electrons and therefore don’t cause interference in the body. Ceramic is also very friendly to the body’s tissues. Unlike metal materials, the gums are able to grow properly around ceramic, which heals well in the bone and accumulates less plaque. This, in turn, helps to counteract inflammation.
So when is the best time to place an implant?
When a tooth needs to be removed, a dentist usually has to wait a while for the wound to heal before filling the gap with an implant. But it turns out that doing the opposite is actually much more effective. Once the tooth is out, it’s best to insert the implant immediately ensuring that the bone and soft tissues are supported right away. It also means the gum doesn’t recede. An implant acts like a kind of plug that supports the tooth socket and bone.
In addition, the body’s regeneration capacity is at its highest when the tooth is removed, since the body is trying to heal the wound anyway. At this time, there are more growth factors being released and protein synthesis is running at full speed. The body also has to rebuild fewer bones this way, because the implant takes up a certain amount of space itself. If there is an extended period of time between the tooth extraction and implant insertion, it’s often the case that valuable bone substance is lost and has to be rebuilt.
Summary
Biological dentistry is the overlap of functional medicine, biohacking, and high tech dentistry—and in my opinion the missing link to overall health.
The “Health Starts In Your Mouth” concept is designed with the focus on optimal health that starts in your oral cavity (as the entrance to your mouth) and addresses chronic inflammation, toxicity, the microbiome, dysbiosis, chronic stress, electrosensitivity, and leaky gum and gut.
At my practice, we prepare the patient for their “health optimization week” with the right food design, which is based on avoiding food intolerances and toxins like grains, sugar, dairy, and highly refined omega-6 oils. The right macronutrient timing and micronutrient tuning (Bone Healing Protocol) help our patients to get out of chronic sympathetic mode (being catabolic).
The goal is to have a strong immune and nervous system that works in balance and isn’t blocked or overly aggressive. This will result in the patient becoming more anabolic, and therefore better able to better build bone and tissue and allow their body to detoxify optimally.
Our experience has shown that when we remove all dental issues like metals, osteonecrosis in the jaw bone (FDOJ/CIBD/NICOs/cavitations), root canals, and other interference fields, the immune and nervous system will finally start to work optimally again, and as a bonus will be able to osseointegrate ceramic implants. The future starts now and our common goal in functional medicine is optimal health! Remember that health starts in your mouth.
For more information, or to find a holistic dentist in your area, check out the following resources:
- International Academy of Oral Medicine & Toxicology
- International Academy of Ceramic Implantology
- International Society of Metal-Free Implantology
And of course, there's plenty more on this topic available in my book It's All in Your Mouth: Biological Dentistry and the Surprising Impact of Oral Health on Whole Body Wellness.
Please leave any comments, questions, or thoughts below, and I'll be happy to get back to you!


HOW EXERCISE HELP IN REACHING GOALS
So the most Frequent question is here how exercise help to reach your goals, Top Facts to reach your goals, Visit my website for more fitness blogs.
For more information click on the link.
I love your your doing to help your audience out during this tough time. although if you want some extra tools and information for diets you can review my custom keto diet if you want.
Love the information. My wife just had a ceramic implant. When it was put in, the Dr. warned us that it has a lower success rate than titanium. Well…the implant failed and the Dr. took it out. We don’t know what to do now. In placing a ceramic implant, does the Dr. need to have special skills in doing so? Our Dr. said that he’s done it before and had success, but prefers titanium due to the higher success rate. The whole ordeal was traumatic for her and we don’t know what to do now. The other options, like bridge doesn’t seem desirable as well as it damages the neighboring teeth. We can’t find a biological dentist near us, any advice would be appreciated. We’re leaning towards leaving it alone and having a denture rather than going the traditional route. Willing to travel if we find the right Dr.
Love the article- excellent information, however, wish you would’ve included the benefits of airway centered dentistry- palate expansion, myofunctional therapies for tongue training, etc to grow our collapsed airways due to generational nutritional injury. What is your oral appliance strategy for growing your patient’s airway? Would love to hear your thoughts!
What about permanent retainers that were placed in the mouth following orthodontia? Obviously, this would be classified as a metal in the mouth, but are there ceramic/alternate materials that could be used?
I have a retainer and have the same question. I am also worried about it constantly leaching chemicals every night in my mouth.
Would like information on that as well…
When it comes to fillings, is “composite” the same as ceramic?